Healthcare Utilization and Costs of Liver Transplantation for Alcoholic Hepatitis
1Medicine, Liver Diseases, Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, RMTI, New York, NY, 2Surgery, Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, RMTI, New York, NY, 3Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, RMTI, New York, NY
Meeting: 2020 American Transplant Congress
Abstract number: A-170
Keywords: Alcohol, Economics, Length of stay, Liver transplantation
Session Information
Session Name: Poster Session A: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: To determine the healthcare utilization and costs of a liver transplantation (LT) for severe alcoholic hepatitis (AH) program.
*Methods: We performed a retrospective healthcare utilization and cost analysis of a prospectively maintained database of hospitalized patients with AH and all inter-hospital transfers (including acute on chronic liver failure, ACLF) at our center from 6/2011-6/2016. ACLF was defined by EASL-CLIF definition. The hospital finance accounting system determined the actual hospital cost of LT admission. Fee schedules for Medicare DRGs 005/432 and a large insurance company were examined to determine expected payments in 2016, including cases exceeding the Medicare outlier threshold and compared to our accounting data.
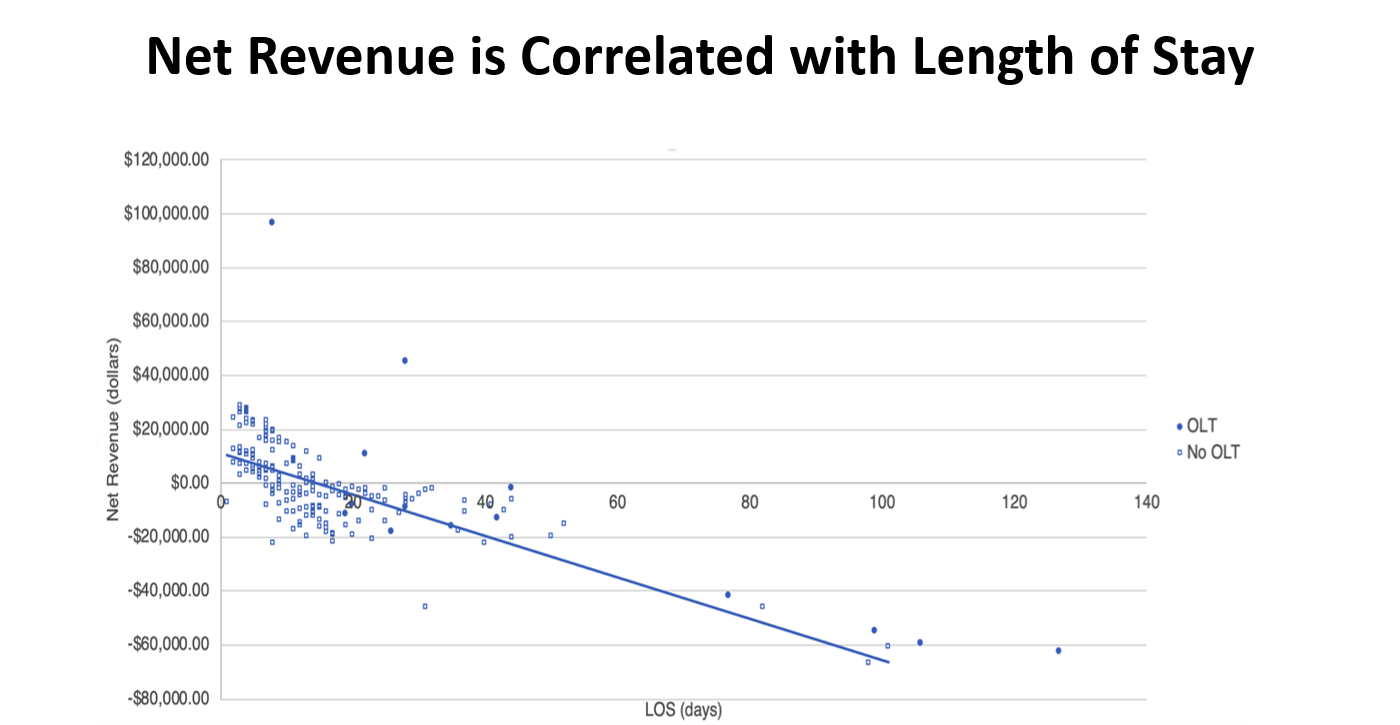
*Results: Over the 5-year study period, 190 patients with severe AH (median DF 77, MELD 31) were hospitalized at our center with 74% arriving via interhospital transfer. A total of 169 (89%) patients were non-responders to steroids and considered for LT. The majority were declined for LT due to unfavorable psychosocial (n=125, 89%) or medical profiles. Out of 27 patients listed for LT for AH, 16 (10%) LT were performed. Insurance coverage was 52% private, 48% public. Average hospital costs of admission for LT for AH and AH without LT were $279,473 and $26,241, respectively. The LT group had a net revenue loss of $42,723 per patient, while the AH without LT group had a net gain of $1,254 per patient. Organ acquisition costs accounted for about one-third of resource use in the LT group. The 5-year net revenue of our LT for AH program was -3% and similar to our LT for ACLF program (-7%, p=0.37). Length of stay (LOS) was high in LT group versus without LT, 35 v 11 days, (p<0.001). LOS was a key driver of cost compared to MELD and >10 other variables, with a strongly negative correlation with net revenue (r= -0.719, p<0.001), Figure 1.
*Conclusions: Healthcare utilization of LT for AH is extensive with only 10% selected and surviving to LT. Costs were high and influenced by LOS. An evidence-based, selective strategy of LT for AH yields negative, but near neutral net revenue. Reduction of LOS in LT for AH, rather than higher volume will improve center financial viability. The 5-year net revenue of LT programs for AH and ACLF, a more widely accepted indication for LT, are similar.
To cite this abstract in AMA style:
Im G, Vogel A, Florman SS, Aqui S, Kim-Schluger L, Schiano T. Healthcare Utilization and Costs of Liver Transplantation for Alcoholic Hepatitis [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/healthcare-utilization-and-costs-of-liver-transplantation-for-alcoholic-hepatitis/. Accessed March 7, 2026.« Back to 2020 American Transplant Congress