Healthcare Resource Utilization for Patients with Donor-Specific Antibodies Post-Kidney Transplantation.
1Northwestern University Transplant and Outcomes Research Collaborative (NUTORC), Chicago
2Astellas Pharma Global Development, Northbrook
3Now with UCB, Atlanta
4Dept of Preventive Medicine, Northwestern University, Chicago
Meeting: 2017 American Transplant Congress
Abstract number: B148
Keywords: Alloantibodies, HLA antibodies, Kidney transplantation, Resource utilization
Session Information
Session Name: Poster Session B: Kidney Complications II
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Formation of de novo donor-specific antibodies (dnDSA) against human leukocyte antigens (HLA) contributes to inferior kidney transplant (KT) outcomes. No data exist on healthcare resource utilization (HCRU) of patients developing dnDSA post-transplant. We assessed the effect of DSA on inpatient/outpatient HCRU in the largest single-center KT cohort to date.
Demographic, graft and patient data were collected for all adult KT patients (2007–2015). DSA was assessed at transplant (time 0), 3 and 6 months, 1 and 2 years, and for cause. Patient groups: no dnDSA, dnDSA, and DSA at KT. HCRU, including number of biopsies/emergency department (ED) and inpatient/outpatient visits were abstracted from the Northwestern Medicine Enterprise Data Warehouse.
1517 KT patients [mean age (standard deviation): 49.5 years (13.2), 63.1% male] were followed for ≤8 years (mean 4.4). Patient demographics: Figure 1.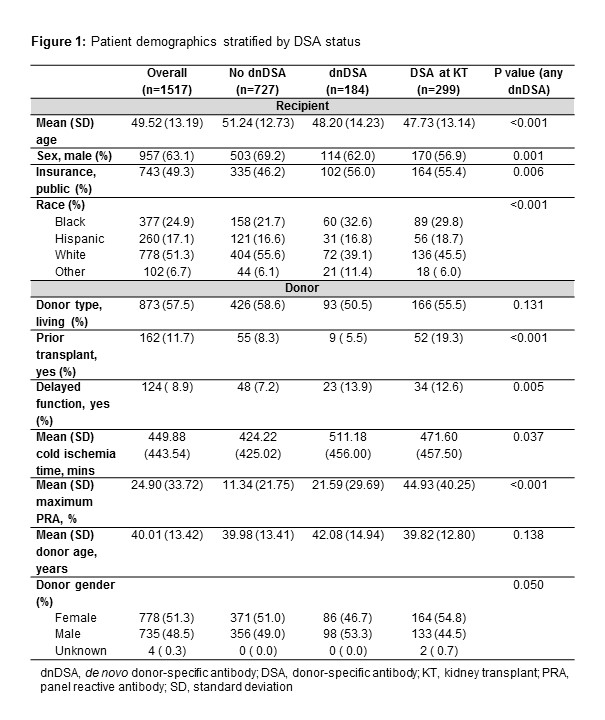 Poisson regression by HLA class/locus showed number of biopsies, ED encounters and inpatient/outpatient visits were significantly greater in patients with dnDSA or DSA at KT vs no dnDSA. Median counts with no dnDSA, dnDSA, and DSA at KT (all classes/loci): biopsies 1, 2 and 1; ED visits 0, 1 and 1; hospitalization 3, 5 and 4; outpatient visits 32, 42 and 47 (p<0.001) (Figure 2).
Poisson regression by HLA class/locus showed number of biopsies, ED encounters and inpatient/outpatient visits were significantly greater in patients with dnDSA or DSA at KT vs no dnDSA. Median counts with no dnDSA, dnDSA, and DSA at KT (all classes/loci): biopsies 1, 2 and 1; ED visits 0, 1 and 1; hospitalization 3, 5 and 4; outpatient visits 32, 42 and 47 (p<0.001) (Figure 2).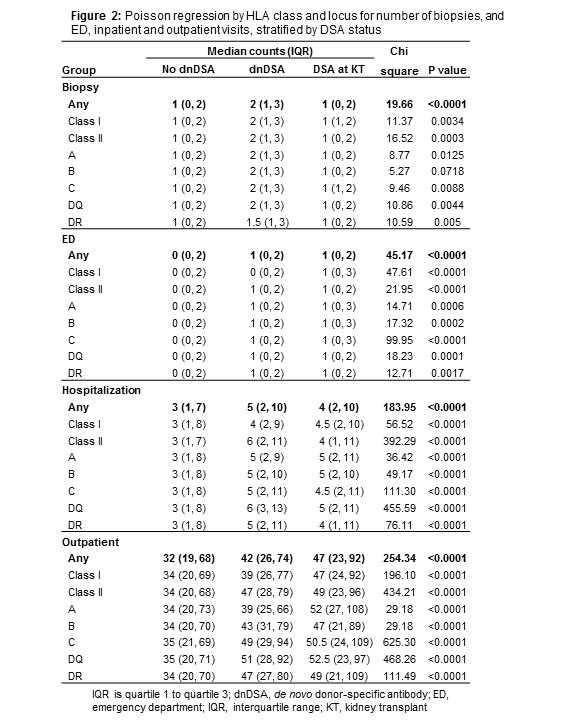 Irrespective of clinical presentation, presence of DSA at KT or development of dnDSA predisposes to increased HCRU following KT. This is noteworthy for inpatient/outpatient visits but does not differ based on HLA class/locus. Minimizing DSA formation has implications for those managing transplant patients.
Irrespective of clinical presentation, presence of DSA at KT or development of dnDSA predisposes to increased HCRU following KT. This is noteworthy for inpatient/outpatient visits but does not differ based on HLA class/locus. Minimizing DSA formation has implications for those managing transplant patients.
CITATION INFORMATION: Ho B, Bhagat H, Lee E, Atiemo K, Daud A, Kang R, Montag S, Zhao L, Schwartz J, Ladner D. Healthcare Resource Utilization for Patients with Donor-Specific Antibodies Post-Kidney Transplantation. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ho B, Bhagat H, Lee E, Atiemo K, Daud A, Kang R, Montag S, Zhao L, Schwartz J, Ladner D. Healthcare Resource Utilization for Patients with Donor-Specific Antibodies Post-Kidney Transplantation. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/healthcare-resource-utilization-for-patients-with-donor-specific-antibodies-post-kidney-transplantation/. Accessed March 3, 2026.« Back to 2017 American Transplant Congress
