Health and Economic Disparities in Waitlist Access and Liver Distribution Policy
1Surgery, Emory University, Atlanta, GA
2Hepatology, University of Pennsylvania, Philadelphia, PA.
Meeting: 2018 American Transplant Congress
Abstract number: 354
Keywords: Economics, Liver cirrhosis, Liver transplantation, Waiting lists
Session Information
Session Name: Concurrent Session: Liver: MELD, Allocation and Donor Issues - 1
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: Room 6B
Background:Sociodemographic disparities compound mortality on the liver transplant waitlist, but the relevance of waitlist disparities to mortality and access among the general population remains unclear.
Methods: US Census, Centers for Disease Control and Prevention and Scientific Registry of Transplant Recipients from 2002-2015 were used. Sociodemographic disadvantage was assessed by Community Health Score (CHS), rural/urban classification, median household income, proportion of adults living in poverty, and percent of adults who are uninsured. Comparisons were made of adult disease prevalence by waitlist additions and deaths and general population end stage liver disease (ESLD) deaths.
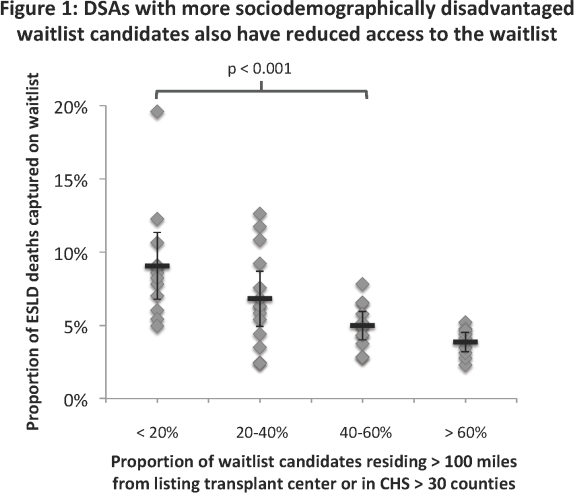
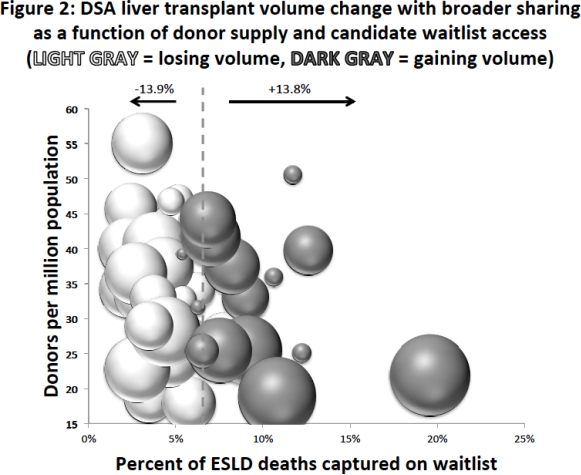
Results: There were 477,595 ESLD and 31,487 waitlist deaths. Higher CHS, higher rates of poverty and uninsurance, rural residence and lower median income were all correlated with increased ESLD mortality and lower waitlist access (p < 0.001 for each trend.) Donor Service Areas (DSAs) with higher proportions of candidates living remotely or in high-CHS counties had lower waitlist rates (Figure 1). Aggregate modeled change to DSA-level transplant volume across all publicly available UNOS proposals in the last two years showed stronger association with waitlist access than donor productivity (Figure 2, dotted line indicates national mean for access).
Conclusions: Adverse local health and economic conditions are associated with reduced access to the transplant waitlist. Sociodemographic disparities impacting candidate waitlist mortality are concentrated in the same DSAs with the lowest levels of waitlist access. Proposals for broader liver sharing that use MELD disparity as an equity measure predominantly shift organs away from areas with more vulnerable patients and reduced waitlist access.
CITATION INFORMATION: Lynch R., Ross K., Pearson T., Goldberg D., Patzer R. Health and Economic Disparities in Waitlist Access and Liver Distribution Policy Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Lynch R, Ross K, Pearson T, Goldberg D, Patzer R. Health and Economic Disparities in Waitlist Access and Liver Distribution Policy [abstract]. https://atcmeetingabstracts.com/abstract/health-and-economic-disparities-in-waitlist-access-and-liver-distribution-policy/. Accessed March 5, 2026.« Back to 2018 American Transplant Congress