Harnessing Scientific and Technological Advances to Improve Equity in Kidney Allocation Policies.
1Agence de la Biomedecine, Saint Denis, France
2Saint Louis Hospital, Paris, France
3Northwestern University, Chicago
Meeting: 2017 American Transplant Congress
Abstract number: 123
Keywords: Allocation, Histocompatibility
Session Information
Session Name: Concurrent Session: Kidney Allocation: Changes and Consequences
Session Type: Concurrent Session
Date: Sunday, April 30, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: E450a
To increase the likelihood of finding a compatible donor, kidney allocation systems prioritize highly sensitized patients to counterbalance the impact of HLA allo-sensitization and preclude organ offers to patients with donor-specific-antibodies. We have shown that precise definition of HLA-DQ assignment can be enhanced by viewing HLA-DQ molecules as combinations of alpha and beta chains.
In this simulation study we evaluated the impact of incorporating HLA-DQ antigens and antibodies as the A/B and αβ allelic variants, respectively, on calculated PRA and probability of finding a compatible donor.
A cohort of 1162 donors (high resolution typed for HLA-DRB/DQA/DQB) and 2075 sensitized candidates in the Ile de France district (with at least one HLA-DQ antibody at >1000MFI, using luminex raw data) was used to compute allelic cPRA and the number of potential compatible donors (PCD) using HLA-DQαβ “allelic” (study) versus “serologic” (current practice) nomenclature.
A significant (p<10-4) decrease in cPRA was observed for the overall population. Sub-analysis demonstrated a higher impact for male versus female, and first transplant versus re-transplant (p<10-4). No impact was observed within each blood group. Interestingly, the population that showed the most change in cPRA was patients with moderate levels of cPRA (30-80%). More importantly, calculating how redistribution of cPRA affects allocation points in the new UNOS-KAS – a decrease of 37% in patients qualifying for the 100% cPRA status was observed. Using allelic versus serologic nomenclature for HLA-DQ also had a significant effect on the number of PCD for all patients. Similar to cPRA calculation, male and first-transplant patients saw a higher increase in PCD compared with female and re-transplants. Last, patients from all blood groups saw an expansion of PCD, with patients of blood group O showing the most benefit.
Our simulation study provides strong support for the need to re-evaluate how HLA-DQ antigens and antibodies are incorporated into allocation policies to ensure equity.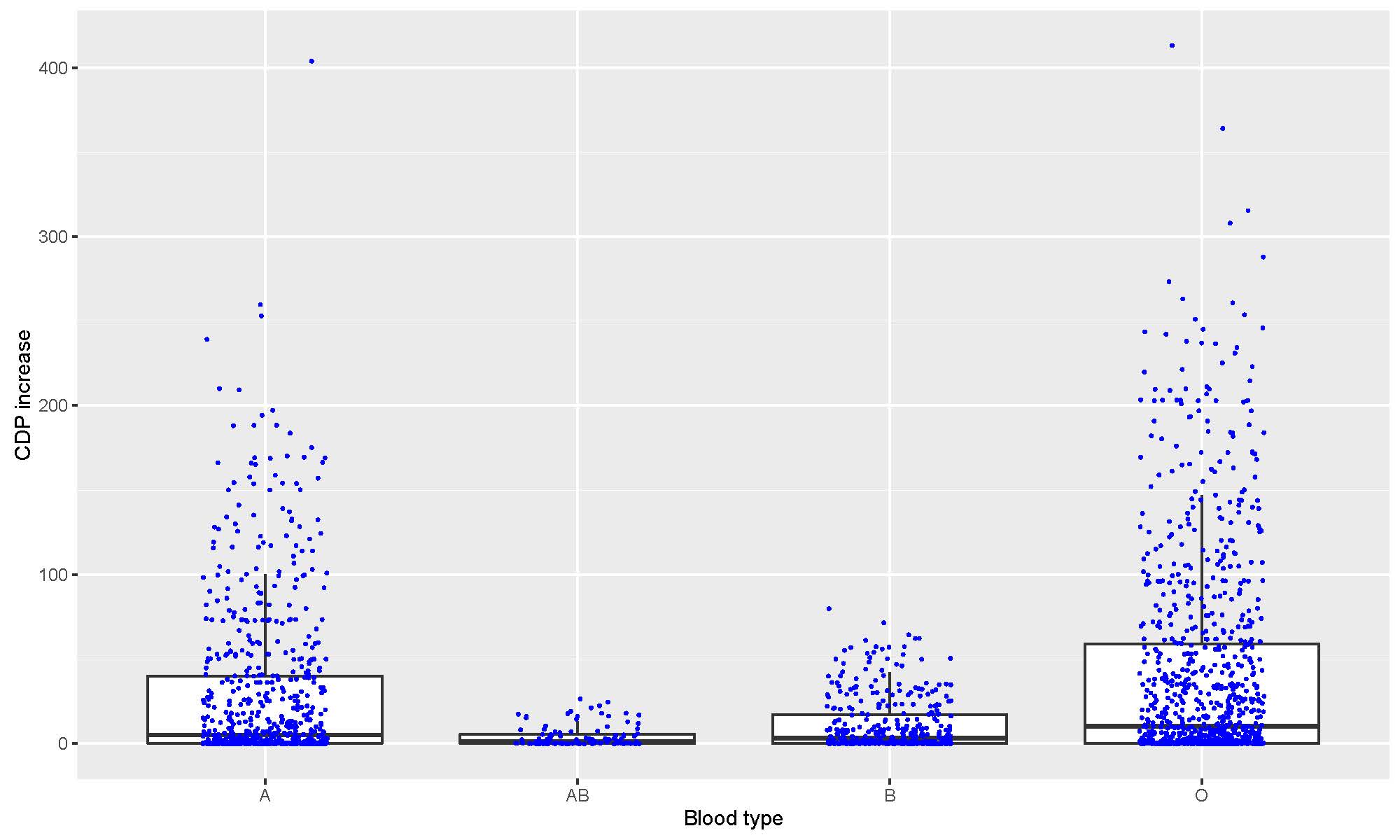
CITATION INFORMATION: Jacquelinet C, Audry B, Antoine C, Suberbielle C, Glotz D, Tambur A. Harnessing Scientific and Technological Advances to Improve Equity in Kidney Allocation Policies. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Jacquelinet C, Audry B, Antoine C, Suberbielle C, Glotz D, Tambur A. Harnessing Scientific and Technological Advances to Improve Equity in Kidney Allocation Policies. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/harnessing-scientific-and-technological-advances-to-improve-equity-in-kidney-allocation-policies/. Accessed March 3, 2026.« Back to 2017 American Transplant Congress
