Growing LDLT Volumes at a US Center- What Does It Take to Do Over 100 LDLTs Per Year
A. Humar, C. Hughes, G. Mazariegos, K. Soltys, A. Gallatin, K. Emmett, A. Tevar, M. Molinari, A. Ganoza, V. Gunabushanam, S. Ganesh
University of Pittsburgh, Pittsburgh, PA
Meeting: 2021 American Transplant Congress
Abstract number: 430
Keywords: Liver, Living donor, Living-related liver donors
Topic: Clinical Science » Liver » Liver: Living Donor Liver Transplant and Partial Grafts
Session Information
Session Time: 7:30pm-8:30pm
 Presentation Time: 8:00pm-8:10pm
Presentation Time: 8:00pm-8:10pm
Location: Virtual
*Purpose: LDLT remains underutilized in the US, accounting for <6% of the annual total liver transplant volume. We examined methods we have incorporated to expand LDLT volume at our center.
*Methods: Data was collected on all donors and recipients that underwent LDLT at our center, looking at the impact of various programs on total volumes.
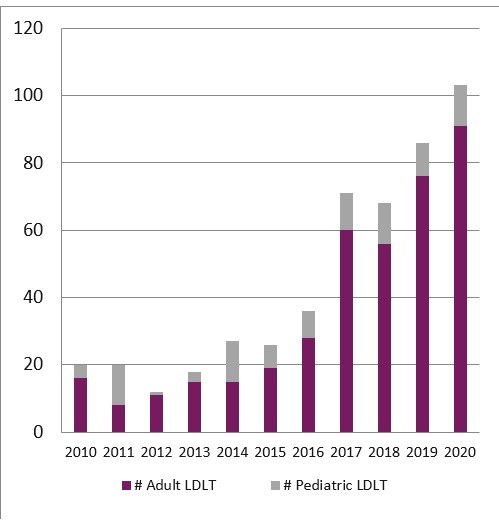
*Results: LDLT remains underutilized in the US, accounting for <6% of the annual total liver transplant volume. We have made a concerted effort to grow LDLT at our program and it now represents 60% of our annual total adult liver transplant volume and 40% pediatric total volume. In 2020, we will perform >100LDLTs at our program (91 adults, 12 pediatric, Figure1). Growth in volume has been due to many factors, including a change in our philosophy to consider an LDLT as the 1st and best option for the vast majority of our patients. We utilized paired exchanges (6 pairs, 12 transplants), ABO incompatible donors (n=1), as well as non-directed donors (n=13) to maximize donor acceptance and utilization. Our donor acceptance rate is 70%, with our most common reason for donor exclusion being steatotic liver or psychosocial factors. We have excluded very few donors based on GW/RW ratio; 11% of the adult transplants had GW/RW<0.8%. We have utilized extensive education programs, targeted for individual recipients as well as for the general public to raise awareness regarding LDLT. All recipients are seen by the LD team and are offered programs such as our Champions program to help them identify suitable living donors. For recipient selection, MELD- either at the upper or lower end- are not considered contraindications to LDLT. We also offer LDLT to recipients who may not qualify for a deceased donor, but we know are likely to have a better outcome with liver transplant vs best other therapy. This includes patients with HCC beyond Milan, cholangiocarcinomas (hilar and intrahepatic, n=2), metastatic colorectal cancers (n=2), as well as other expanded indications. Despite expanded indications, results have been acceptable. All donors are well with 2 early bile leaks (both managed non-operatively), and 3 reoperations (1 bleeding, 1 SBO, 1 incisional hernia). No donor required blood transfusion. Recipient graft and patient survival is 95% and 96% in the adult patients. Survival has been 100% in the pediatric patients.
*Conclusions: Utilization of LDLT can be safely expanded as programs gain more comfort level and experience with the procedure.
To cite this abstract in AMA style:
Humar A, Hughes C, Mazariegos G, Soltys K, Gallatin A, Emmett K, Tevar A, Molinari M, Ganoza A, Gunabushanam V, Ganesh S. Growing LDLT Volumes at a US Center- What Does It Take to Do Over 100 LDLTs Per Year [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/growing-ldlt-volumes-at-a-us-center-what-does-it-take-to-do-over-100-ldlts-per-year/. Accessed February 18, 2026.« Back to 2021 American Transplant Congress