Graft Survival in Sensitized and Non-Sensitized Patients: Role of the Combination of Donor-Specific Antibodies and Acute Rejection.
1Renal Transplant Service, Hospital das Clínicas de São Paulo, Sao Paulo, Brazil
2Immunology Laboratory, Instituto do Coração (InCor), Sao Paulo, Brazil.
Meeting: 2016 American Transplant Congress
Abstract number: D29
Keywords: HLA antibodies, Kidney transplantation, Rejection, Survival
Session Information
Session Name: Poster Session D: Antibody Mediated Rejection: Session #2
Session Type: Poster Session
Date: Tuesday, June 14, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Background: Sensitized (S) patients have higher risk for acute rejection (AR), especially ABMR. DSA is a risk fator for ABMR, however, its impact on AR incidence within 1st post-Tx year remains controversial. The aim is to evaluate graft (GS) and patient survival (PS) in non-sensitized and sensitized patients (pts) according to AR occurrence in pts receiving tacrolimus and mycophenolate as immunossupression.
Methods: Unicentric, retrospective study including 1002 isolated kidney recipients > 18yo transplanted between Jan/09-Dec/2013. They were followed for 35mo (12-60mo). Pre-Tx DSA (A/B/DR) was analyzed by single antigen bead and AR by Banff'09. Results: From 1002 pts, 15 had no DSA performed and were excluded. 937 enrolled: majority were male (57%), 1st Tx (93%), blood transfusion (BT, 53%), pregnancies (74%), deceased donor (63%) and 41% Thymoglobulin as induction. Were subclassified according to pre-Tx calculated PRA as: 744 (75%) non-sensitized (NS;PRA=0%) and 26% (243) sensitized (S;PRA≥1%). Among S pts, 37.5% (91) were pre-Tx DSA+ while 62.5% (241) were DSA–. Overall 1st year AR incidence was 14.4% (144: 70% TCMR/30% ABMR). All groups had ABMR and T-Cell mediated (TCMR) AR: NS 11% (76TCMR/6ABMR), DSA– 15% (16TCMR/7ABMR) and DSA+ 43% (8TCMR/31ABMR), p<0.0001. ABMR more frequent in pre-Tx DSA+ pts, p<0.0001 and was associated with previous Tx (OR 15, p<0.0001), BT (OR 2.718, p=0.01), female (OR 3.63, p<0.001) and >5 mismatches (OR 2.32, p=0.025) and pre-Tx DSA+ (OR 9.41;p<0.0001). DSA-MFI was similar between AR+ and AR– pts, 4419±3690 vs 3670±2707, p=NS. DSA+/AR+ pts had worse GS when compared to DSA+/AR– and DSA– and NS with or withou AR
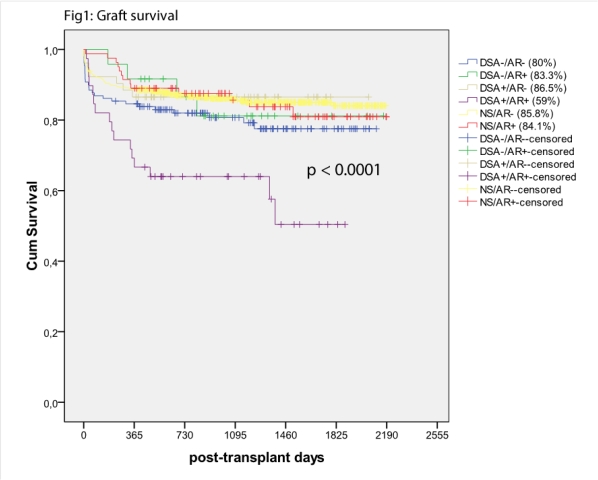
(Fig1). PS was similar in all groups.
Conclusion: Pre-Tx DSA was a risk factor for AR, however DSA level was not a predictor for ABMR. AR occurrence in DSA+ pts strongly impacted on long-term graft survival when compared to DSA+ pts without AR, highlighting the impact of acute rejection on graft survival.
CITATION INFORMATION: Souza P, Aguirre A, Bezerra G, Rodrigues H, Agena F, David D, de Paula F, David-Neto E, Castro M. Graft Survival in Sensitized and Non-Sensitized Patients: Role of the Combination of Donor-Specific Antibodies and Acute Rejection. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Souza P, Aguirre A, Bezerra G, Rodrigues H, Agena F, David D, Paula Fde, David-Neto E, Castro M. Graft Survival in Sensitized and Non-Sensitized Patients: Role of the Combination of Donor-Specific Antibodies and Acute Rejection. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/graft-survival-in-sensitized-and-non-sensitized-patients-role-of-the-combination-of-donor-specific-antibodies-and-acute-rejection/. Accessed March 3, 2026.« Back to 2016 American Transplant Congress
