GLP1-RAs, SGLT2i Are Underutilized in Kidney Transplant Recipients with Diabetes Mellitus and Obesity
M. Stumpf, S. A. Dar, S. Rao, A. Doyle
University of Virginia, Charlottesville, VA
Meeting: 2020 American Transplant Congress
Abstract number: A-062
Keywords: Hyperglycemia, Kidney transplantation, Metabolic complications, Post-transplant diabetes
Session Information
Session Name: Poster Session A: Kidney: Cardiovascular and Metabolic Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: There is little research describing differences in use of antidiabetic medications amongst obese, diabetic patients with or without a history of kidney transplant. More specifically, commonly used oral antidiabetic drugs (OADs) like metformin, GLP1-RA, and SGLT2i have favorable effects on glycemic control and weight loss . We sought to determine the odds ratio of use of OADs amongst obese, diabetic patients with or without a history of kidney transplant.
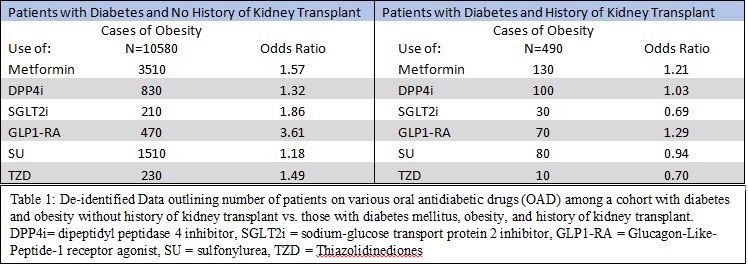
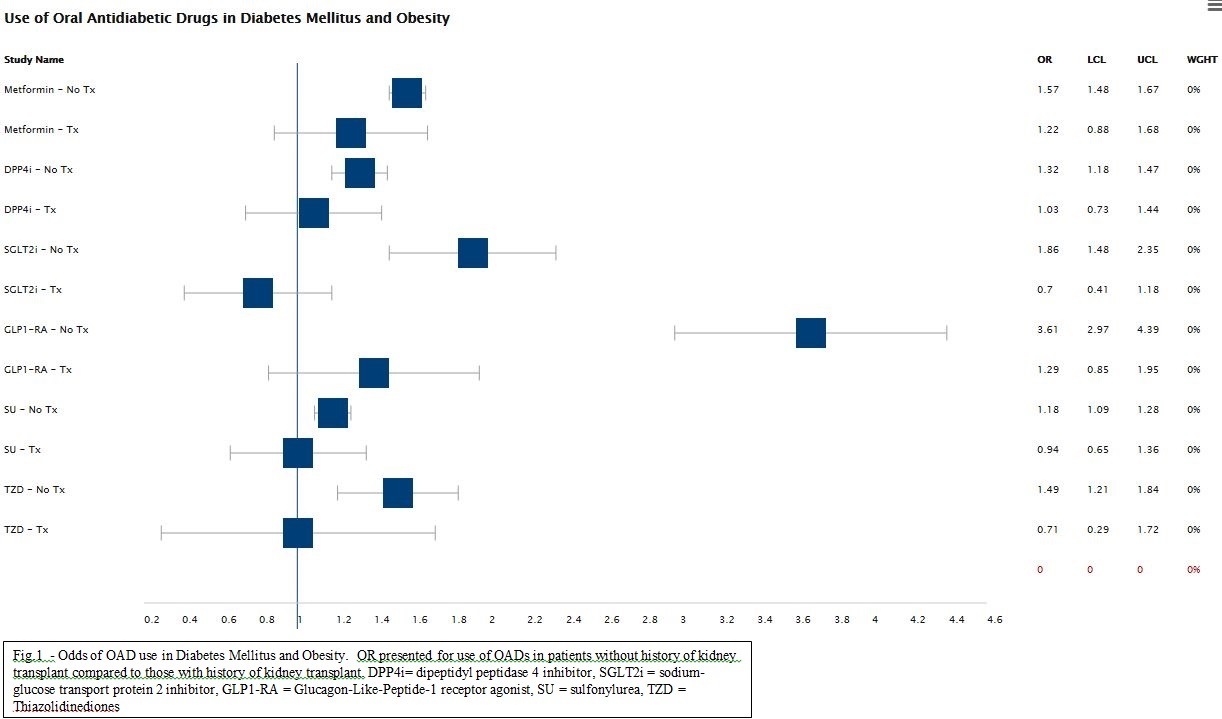
*Methods: This study was cross-sectional in design. A de-identified database was utilized to query for patients (>18yo) seen at a single tertiary medical center with diagnosis code of diabetes mellitus (DM) and either a diagnosis code of obesity or BMI >30 kg/m2 (Cases) vs no obesity (Control). The same query was then conducted to include only patients with diagnosis code of kidney transplant (Table 1). No exclusions were made based on kidney function. Given obesity, an Odds Ratio (OR) was then calculated for use of OADs in both patients with history of kidney transplant and those without (OR = [cases exposed to drug/cases unexposed to drug]/[controls exposed to drug/controls unexposed]).
*Results: ORs were calculated and presented in Figure 1. Metformin use was not significantly different between the two groups (OR without kidney transplant was 1.57 [95%CI 1.48-1.67], OR with transplant was 1.22 [95%CI 0.88-1.68]). However, SGLT2i and GLP1-RA therapy were both significantly less likely to be used in patients who have kidney transplant history. OR of SGLT2i without transplant 1.86 [95%CI 1.48-2.5] vs OR of SGLT2i in transplant 0.69 [95%CI 0.41-1.18]. OR of GLP1-RA without transplant 3.61 [95%CI 2.97-4.39] vs GLP1-RA in transplant 1.29 [95%CI 0.85-1.95].
*Conclusions: Recent advances in therapy for DM include medications which favor weight loss and lend cardiovascular benefit, including GLP1-RA and SGLT2i. These medications are not contraindicated in patients with history of kidney transplant, yet are often not utilized. Further studies are needed to demonstrate safety and efficacy of these agents in patients with diabetes mellitus, obesity, and history of kidney transplant.
To cite this abstract in AMA style:
Stumpf M, Dar SA, Rao S, Doyle A. GLP1-RAs, SGLT2i Are Underutilized in Kidney Transplant Recipients with Diabetes Mellitus and Obesity [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/glp1-ras-sglt2i-are-underutilized-in-kidney-transplant-recipients-with-diabetes-mellitus-and-obesity/. Accessed June 30, 2025.« Back to 2020 American Transplant Congress