Gender Disparity in Living Donor Kidney Transplants
SUNY Downstate Medical Center, Brooklyn, NY
Meeting: 2020 American Transplant Congress
Abstract number: 131
Keywords: Kidney transplantation, Living donor
Session Information
Session Name: Kidney Living Donor: Other I
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: Over the last decades, the number of kidney transplants has increased. However, more male than female patients receive a transplant. While the male/female ratio has remained relatively constant in deceased donor kidney transplants it has changed over time in living donor transplants.
*Methods: This study included all 106,260 primary adult living donor kidney transplants reported to UNOS/OPTN and performed between 1998 and 2018. To account for annual fluctuations, 3-year intervals were assessed. Comprehensive univariate and multivariate analyses were performed to describe changes and risk factors for female living donor kidneys transplants.
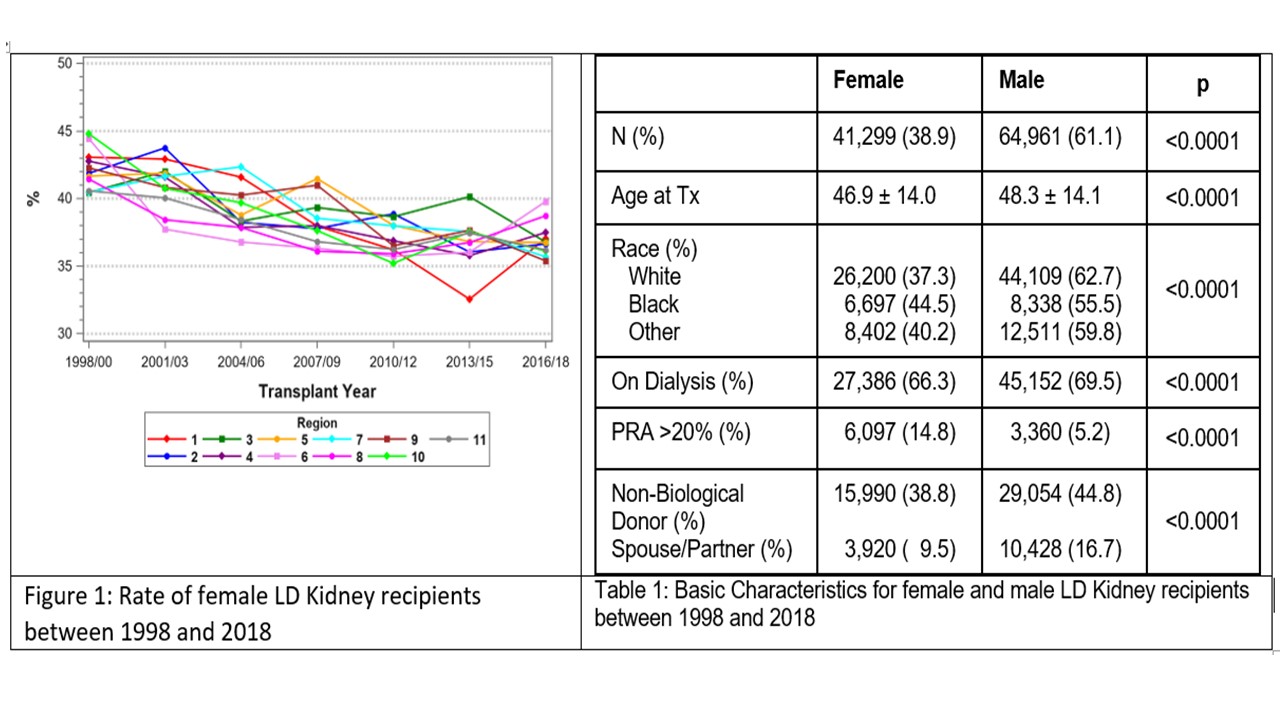
*Results: Table 1 shows the overall basic gender differences. Male recipients were on average older, more likely to be white, more often on dialysis at the time of transplant, and more often recipients of a non-biological donor kidney. Female recipients, in contrast, were significantly more often sensitized. Over time, age of both male and female recipients increased but male recipient age increased more so.
The rate of female LDK recipients declined from 41.94% in 1998/2000 to 36.68% in 2016/18. This means a change in absolute disparity from 16% to 27%. Figure 1 shows the consistent significant decline by UNOS region . The decline was confirmed in our multivariate analysis (p<0.001). The likelihood to receive a LDK declined for women with increasing age and the odds to receive a LDK kidney was higher for a black than for a white woman. Also, the odds to receive a kidney from a non-biological donor was significantly lower for women. Over time, significantly more female spouses donated a kidney to their husband. The odds for a LDK were only significantly increased for sensitized women. In case of sensitization, the rate of non-biological donors increased in women as it did in men.
*Conclusions: (1) the disparity of receiving a LDK has continued to increase over time in favor of men; (2) the likelihood to receive a LDK kidney was higher for a black vs white woman; (3) the likelihood to receive a LDK from a non-biological donor (spouse) was significantly lower for women vs men; (4) only the likelihood to receive a LDK was higher for sensitized women vs men. Gender disparity in 2019/20 remains real in LDK transplantation.
To cite this abstract in AMA style:
Gruessner A, Saggi S, Renz J, Markell M, Salifu M, Gruessner R. Gender Disparity in Living Donor Kidney Transplants [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/gender-disparity-in-living-donor-kidney-transplants/. Accessed July 12, 2025.« Back to 2020 American Transplant Congress