FSGS Recurrence and Graft Survival in Pediatric Renal Transplants: A NAPRTCS Registry Analysis
1Starship Children's Health, Auckland, New Zealand
2EMMES Corp., Rockville
3BC Children's Hospital, Vancouver, Canada.
Meeting: 2018 American Transplant Congress
Abstract number: B208
Keywords: Graft survival, Kidney transplantation, Nephrotic syndrome, Recurrence
Session Information
Session Name: Poster Session B: Kidney: Pediatrics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Introduction
Previous studies have raised concern of adverse outcome of living donor (LD) grafts in children transplanted for FSGS. This study reassesses impact of donor source, immunosuppression and baseline features on graft survival in a contemporary cohort from the NAPRTCS.
Methods
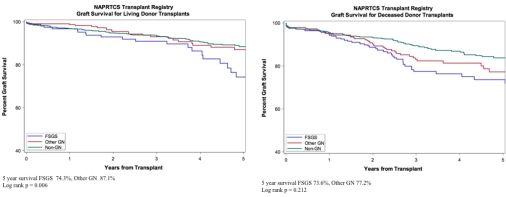
Using the NAPRTCS registry, outcomes were compared between FSGS, non-FSGS glomerulopathies (GN) and non-glomerular kidney diseases (non-GN). 3010 transplants occurred between 2002-2017. 455 had FSGS, 690 had GN and 1865 had non-GN. Median follow-up time was 2.5 years (0.0-14.3 years). Primary outcome was graft survival, including death with function. Secondary outcomes included patient survival and acute rejection. We used Kaplan-Meier estimates of graft survival, acute rejection and patient survival. Mutivariable Cox regression models described relative risks of graft failure (GF).
Results
FSGS and GN shared features of older age and more frequent native nephrectomy. The FSGS group had a higher proportion with African American race and deceased donor (DD) graft. More non-GN patients received a preemptive transplant. Induction and primary immunosuppression did not differ between the FSGS and GN groups. A higher proportion of FSGS than GN patients had delayed graft function (DGF) (14.1% vs 8.3%). There was significant difference in survival rates between LD grafts of FSGS and non-FSGS GN patients (HR 1.76, p= 0.016). Survival rates between LD grafts and DD grafts in patients with FSGS were similar (HR 1.46, 0.86 – 2.46, p=0.161). GF was most commonly from recurrence disease in FSGS (42.9%) compared with GN and non-GN (6.9 % and 1%). Associated findings with GF from FSGS recurrence were DGF (HR 7.33, p<0.001), while all-cause GF in FSGS patients was associated with prior transplant (HR 1.94, p=0.014) and DGF (HR 4.39, p<0.001).
Conclusion
The FSGS cohort had reduced LD rates for kidney transplantation, with loss of LD graft survival advantage. Graft failure risk was increased in cases with DGF or re-transplant.
CITATION INFORMATION: Koh L., Martz K., Blydt-Hansen T. FSGS Recurrence and Graft Survival in Pediatric Renal Transplants: A NAPRTCS Registry Analysis Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Koh L, Martz K, Blydt-Hansen T. FSGS Recurrence and Graft Survival in Pediatric Renal Transplants: A NAPRTCS Registry Analysis [abstract]. https://atcmeetingabstracts.com/abstract/fsgs-recurrence-and-graft-survival-in-pediatric-renal-transplants-a-naprtcs-registry-analysis/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress