Frailty, Inflammation, and Waitlist Mortality among Patients with End-Stage Renal Disease
1JHU, Baltimore
2UMich, Ann Arbor.
Meeting: 2018 American Transplant Congress
Abstract number: B113
Keywords: Inflammation
Session Information
Session Name: Poster Session B: Kidney Deceased Donor Allocation
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background: Among older adults, frailty is associated with heightened inflammation and subsequent mortality. Although frailty is common among patients on the KT waitlist, the role of frailty and inflammation in this population remains unclear. We quantified the association between frailty, inflammation, and waitlist mortality and tested whether frailty and/or inflammation improves risk prediction beyond registry-based factors.
Methods: We studied 1,975 prevalent ESRD patients on the KT waitlist (11/1/09-2/28/17) in a multi-center cohort study of patients undergoing KT evaluation; serum inflammatory markers (interleukin-6 [IL-6], soluble tumor necrosis factor-a receptor-1 [sTNFR1], and C-reactive protein [CRP]) were analyzed in 605 of these participants. We compared the C-statistic of an established registry-based prediction model adding frailty and/or inflammation (1SD change in log IL-6, sTNFR1, CRP, or an aggregate inflammatory index).
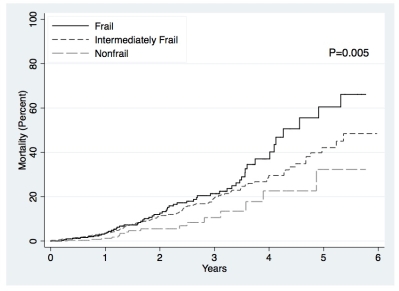
Results: The mean age was 53.7 and 18.4% were frail. Frail candidates had elevated serum IL-6 (P<0.001), sTNFR1 (P=0.02), CRP (P=0.01), and a higher inflammatory index (P<0.001). The registry-based model had moderate predictive ability (C-statistic=0.655). Frailty was associated with increased mortality risk (frail HR=2.19, 95%CI:1.26-3.79) but did not improve mortality risk prediction (C-statistic=0.646; P=0.65). Like frailty, IL-6 (HR=2.13, 95%CI:1.41-3.22), sTNFR1 (HR=1.70, 95%CI:1.12-2.59), CRP (HR=1.68, 95%CI:1.06-2.67), and the inflammatory index (HR=2.09, 95%CI:1.38-3.16) were all associated with increased mortality risk. But unlike frailty, adding IL-6 (C-statistic=0.777; P=0.02), CRP (C-statistic=0.728; P=0.02), or the inflammatory index (C-statistic=0.777; P=0.02) substantially improved mortality risk prediction.
Conclusions: Among patients on the KT waitlist, frailty and inflammation were associated with increased waitlist mortality risk, but only inflammatory markers significantly improved risk prediction. Heightened inflammation may be the biological link between frailty and mortality in KT candidates.
CITATION INFORMATION: McAdams DeMarco M., Ying H., Thomas A., Warsame F., Shaffer A., Haugen C., Garonzik Wang J., Desai N., Norman S., Segev D. Frailty, Inflammation, and Waitlist Mortality among Patients with End-Stage Renal Disease Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
DeMarco MMcAdams, Ying H, Thomas A, Warsame F, Shaffer A, Haugen C, Wang JGaronzik, Desai N, Norman S, Segev D. Frailty, Inflammation, and Waitlist Mortality among Patients with End-Stage Renal Disease [abstract]. https://atcmeetingabstracts.com/abstract/frailty-inflammation-and-waitlist-mortality-among-patients-with-end-stage-renal-disease/. Accessed February 20, 2026.« Back to 2018 American Transplant Congress