Fate of 535 Renal Allografts Retrieved from Donors after Cardiac Death and Risk Factors Affecting Long-Term Graft Survival (Single Center Experience during Three Decades), The
Department of Urology, Fujita-Health University, Toyoake, Aichi, Japan
Department of Organ Transplant Surgery, Fujita-Health University, Toyoake, Aichi, Japan
Meeting: 2013 American Transplant Congress
Abstract number: 536
Introduction: The kidneys procured from deceased donors in donation after cardiac death (DCD) hold great potential to expand the donor pool but have not yet been fully utilized, in part because of concerns about graft dysfunction. In this study, the posttransplant outcome of renal allografts recovered from DCD donors is investigated and the risk factors affecting the renal prognoses were analyzed. Methods: From 1979 to the end of Nov. 2012, 535 kidneys were retrieved from 270 DCD donors at our center, using in situ regional cooling technique. Only 49 (9.2%) grafts had discarded and 443 grafts transplanted since 1983 through 2011 were enrolled in this study. The age of the donors and recipients ranged from 0.7 to 75 (mean; 47.6) and from 7 to 72 (mean; 41.7). The warm ischemic time ranged from 1 to 71 minutes (mean; 11.7). The serum creatinine level before cardiac arrest ranged from 0.4 to 5.4 mg/dl (mean; 1.49). All the patients were treated with immunotherapy consiting of calcineurin inhibitos, steroid and other immunosuppressants. For the statistical analysis, Kaplan-Meier method and Log-rank test were used. Results: Following renal transplants, primary non function (PNF) was noted in 27 (6.5%), immediate function (IF) was 58 (13.1%), and DGF was 358 (80.9%). The 1, 3, 5, and 10 year patient survival rates were 97.0%, 92.1%, 90.0%, and 82.9%, respectively. The 1, 3, 5, and 10 year graft survival rates were 86.1%, 75.6%, 68.5%, and 52.8%, respectively.
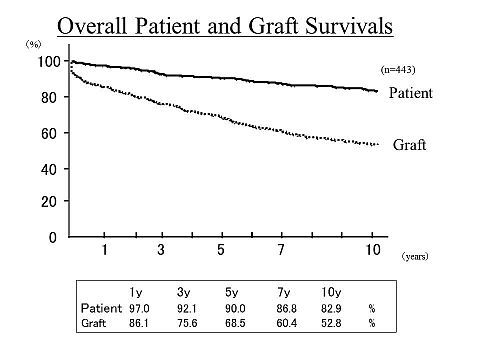
The significant risk factors for graft failure were donor age, cause of death (CVA), donor hypertension and WIT. Conclusion: Renal grafts recovered from DCDs had good renal function as well as excellent long term graft survival, when in situ regional cooling technique was applied. DCD donors should be the excellent resources of deceased donor kidneys, and they can increase the number of renal transplantation in the era of sever organ shortage.
To cite this abstract in AMA style:
Kusaka M, Kubota Y, Takenaka M, Fukami N, Sasaki H, Shiroki R, Kenmochi T, Hoshinaga K. Fate of 535 Renal Allografts Retrieved from Donors after Cardiac Death and Risk Factors Affecting Long-Term Graft Survival (Single Center Experience during Three Decades), The [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/fate-of-535-renal-allografts-retrieved-from-donors-after-cardiac-death-and-risk-factors-affecting-long-term-graft-survival-single-center-experience-during-three-decades-the/. Accessed July 18, 2025.« Back to 2013 American Transplant Congress
