Failure to Account for Social Determinants of Health in Non-HCC MELD Exceptions Exacerbates Geographic Disparities in Access to Liver Transplantation
University of Alabama at Birmingham, Birmingham, AL
Meeting: 2022 American Transplant Congress
Abstract number: 1114
Keywords: Allocation, Liver transplantation, Organ Selection/Allocation, Survival
Topic: Clinical Science » Liver » 60 - Liver: MELD Allocation*
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Non-HCC MELD exceptions have been previously shown to give excess priority for transplant in certain UNOS Regions, but this phenomenon has not been examined on a local level.
*Methods: Adults listed at a single center for primary isolated liver transplant without HCC after June 18, 2013 (start of the previous liver allocation system) in the SRTR database as of March 2021 were examined. Candidates were mapped to hospital referral regions (HRRs) as defined by the Dartmouth Atlas of Healthcare. Waitlist mortality and receipt of a liver transplant were modeled for MELD exception patients vs. patients without exceptions, adjusting for laboratory MELD, era of allocation policy (Share 35 vs. acuity circles), and introduction of the National Liver Review Board, in a time varying manner. Advantaged HRRs were defined as those where exception patients had a statistically higher likelihood of transplant and a statistically similar or lower likelihood of death without transplant. Community health at the HRR level was measured with a modified version of the Robert Wood Johnson Foundation County Health Rankings (CHR). Higher CHRs indicate poorer community health.
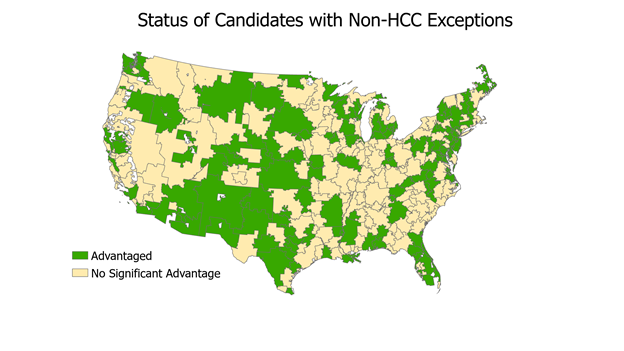
*Results: There were 49,494 candidates in the cohort, of whom 4,336 (8.8%) had MELD exceptions and 45,158(91.2%) did not. Of 304 HRRs, 138 were advantaged (45.4%, figure). The mean CHR of advantaged HRRs was -0.23, vs. 0.19 in non-advantaged HRRs (p=0.008), indicating significantly better community health in these areas. Only 29% of advantaged HRRs were in spatial clusters of high HRR vs. 48.2% of non-advantaged HRRs, while 36.2% of advantaged HRRs were in spatial clusters of low CHR vs.28.3% of non-advantaged HRRs (table).
*Conclusions: Candidates with non-HCC MELD exceptions were significantly advantaged over those without exceptions in nearly half of all HRRs, an advantage associated with significantly better access to care and overall community health outcomes. These findings indicate that assigning the same priority for transplant to all exception candidates without considering social determinants of health may actually exacerbate rather than ameliorate geographic disparity.
| Advantaged Hospital Referral Regions | Non-Advantaged Hospital Referral Regions | |
| High County Health Ranking Clusters | 40 (29.0%) | 80 (48.2%) |
| Low County Health Ranking Clusters | 50 (36.2%) | 47 (28.3%) |
| Non-Cluster Hospital Referral Regions | 48 (34.8%) | 39 (23.5%) |
| p=0.003 |
To cite this abstract in AMA style:
Cannon RM, MacLennan P, Sheikh SS, Orandi BJ, Nasell A, Walker JT, Locke JE. Failure to Account for Social Determinants of Health in Non-HCC MELD Exceptions Exacerbates Geographic Disparities in Access to Liver Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/failure-to-account-for-social-determinants-of-health-in-non-hcc-meld-exceptions-exacerbates-geographic-disparities-in-access-to-liver-transplantation/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress