Factors Predicting Tacrolimus Trough Variability After Lung Transplantation.
The Johns Hopkins Hospital, Baltimore, MD.
Meeting: 2016 American Transplant Congress
Abstract number: B284
Keywords: Drug interaction, Immunosuppression
Session Information
Session Name: Poster Session B: Lung Transplantation Posters
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Background: Recent data suggests that variability in tacrolimus trough concentrations is associated with acute and chronic rejection. The purpose of this study was to identify patient-specific factors present in the post-operative period associated with increased tacrolimus trough variability after lung transplant.
Methods: This was a retrospective cohort study of lung transplant recipients at a large academic medical center from 2011-2015. Tacrolimus trough variability was defined as the standard deviation(SD) of all tacrolimus troughs in a given patient from post-operative days(POD) 8 to 45. Tacrolimus pharmacokinetic studies were reviewed to identify possible factors that may alter absorption or metabolism of tacrolimus and thus potentially influence trough variability. A univariable regression analysis was performed on each factor and those with a p-value of <0.2 were included in a multivariable regression analysis.
Results: A total of 77 patients were included. The overall mean tacrolimus trough and mean tacrolimus trough SD for all patients from POD 8-45 was 10.98±2.2ng/mL and 3.54±1.65ng/mL, respectively. Factors used in the multivariable analysis were: interacting medication at the time of sublingual(SL) to oral tacrolimus conversion, primary diagnosis of cystic fibrosis(CF), use of basiliximab induction, age at time of transplant, ≥2 diet changes during admission, and mean serum creatinine(SCr). A multivariable regression with these factors showed no significant association. However since CF patients were significantly younger and differentially not given induction compared to other diagnoses due to institutional practice, these two variables were excluded from analysis due to colinearity. The resultant model showed a significant association between CF and tacrolimus trough variability(Table 1). 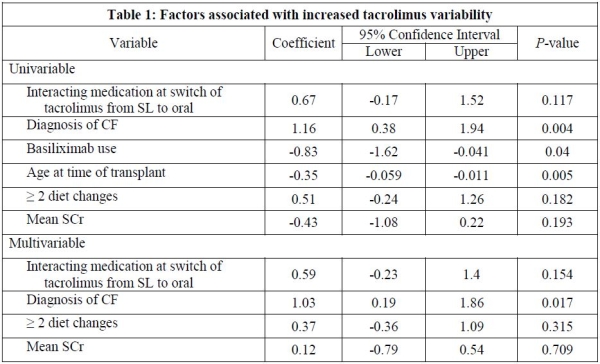
Conclusion: A primary diagnosis of CF was associated with increased tacrolimus trough variability and may reflect either alteration in drug absorption or the younger age typical of this population at the time of transplant. As tacrolimus trough variability has been shown to be associated with allograft dysfunction, practitioners should be vigilant in the management of immunosuppression in this population.
CITATION INFORMATION: Boyle K, Moranville M, Shah P. Factors Predicting Tacrolimus Trough Variability After Lung Transplantation. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Boyle K, Moranville M, Shah P. Factors Predicting Tacrolimus Trough Variability After Lung Transplantation. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/factors-predicting-tacrolimus-trough-variability-after-lung-transplantation/. Accessed July 5, 2025.« Back to 2016 American Transplant Congress
