Evaluation of Risk Factors and Outcomes for Hepatic Artery Thrombosis Post Pediatric Liver Transplantation
1Baylor College of Medicine, Houston, TX, 2Miami Transplant Institute, Miami, FL, 3Texas Children's Hospital, Houston, TX
Meeting: 2020 American Transplant Congress
Abstract number: C-175
Keywords: Hepatic artery, Liver transplantation, Pediatric, Risk factors
Session Information
Session Name: Poster Session C: Liver: Pediatrics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Evaluate which transplantation parameters have an association with HAT, as well as to determine the success rate of HAT intervention at TCH since 2011.
*Methods: This is a retrospective, cross-sectional chart review of pediatric patients with HAT post-PLT performed at Texas Children’s Hospital from January 2011 to March 2019. T-test was used to compare the continuous variables and Person chi-square test was used to compare categorical variable. A p-value of <0.05 was statistically significant.
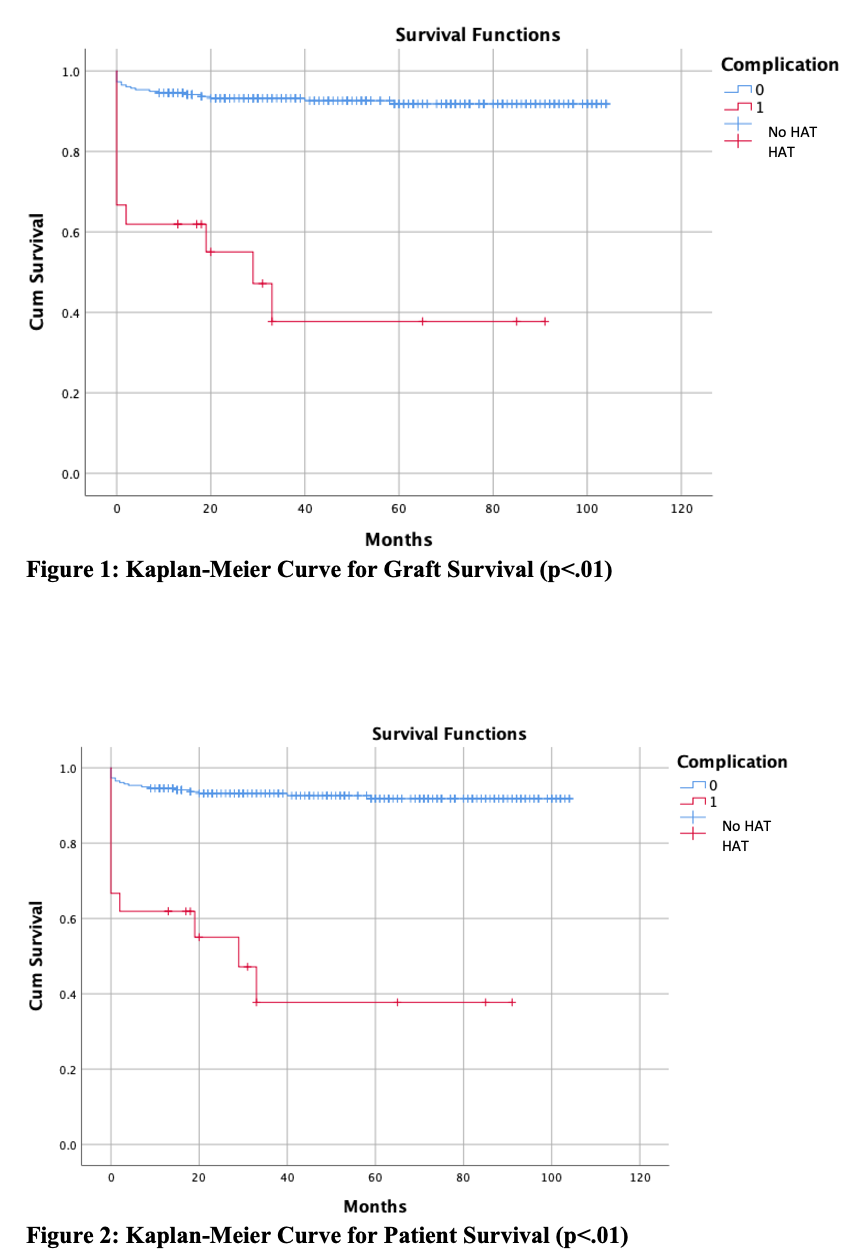
*Results: A total of 284 PTL were performed, with 21 (7.4%) PLTs resulting in HAT. In comparing patients with HAT to without HAT there was not a significant difference in age, weight, gender, disease etiology, donor gender, viral mismatch, wait list time, PELD scores, transplant status, type of transplant and total ischemia time. Difference were found in insurance type, mean donor age, mean donor weight, and pre-transplantation creatinine (Table 1). 30-day graft survival varied between coexisting portal vein thrombosis (33.3%) and without PVT (80%) (p=.04). Restoration of arterial blood flow resulted in 89% (8/9) 30-day graft survival, compared to 50% (6/12) in patients without restored blood flow (p=.061). One-year graft survival for restored blood flow was 78% vs. without restoration was 50%. Results of HAT intervention on restoration of arterial blood flow and patient and graft outcomes are demonstrated in Table 2. Patient and graft overall survival was decreased by HAT (p<.05), see Figure 1 and Figure 2.
*Conclusions: Reducing the risk of HAT and its association with increased morbidity and mortality remains a challenge for future research. Restoration of blood flow was achieved in most cases by IR or surgery and led to significantly improved graft survival.
| HAT (21) | No HAT (263) | P-Value | |
| Insurance (Private) | 62% | 34% | .033 |
| Donor Mean Age (Months) | 5.05 | 9.69 | .051 |
| Donor Mean Weight (kg) | 15.2 | 35.0 | .057 |
| Pre-Transplant Creatinine (mg/dL) | 0.25 | 0.33 | .055 |
| Restoration of Arterial Blood Flow | No Restoration of Arterial Blood Flow | 30-Day Graft Survival w/Treatment | 30-Day Patient Survival w/Treatment | |
| IR | 6/10 (60%) | 4/10 (40%) | 8/10 (80%) | 8/10 (80%) |
| Surgery | 3/5 (60%) | 2/5 (40%) | 4/5 (80%) | 5/5 (100%) |
| Re-Transplant | – | – | – | 6/6 (100%) |
To cite this abstract in AMA style:
McDonald JT, Miloh T, Thompson K, Hosek K, Goss J, Kennedy C. Evaluation of Risk Factors and Outcomes for Hepatic Artery Thrombosis Post Pediatric Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/evaluation-of-risk-factors-and-outcomes-for-hepatic-artery-thrombosis-post-pediatric-liver-transplantation/. Accessed February 18, 2026.« Back to 2020 American Transplant Congress