Epidemiology of Cytomegalovirus (CMV) in Pediatric Solid Organ Transplant Recipients (SOTR) at Texas Children’s Hospital (TCH)
K. Valencia, K. Hosek, E. Moulton, F. Munoz, G. Demmler-Harrison, C. Bocchini
Baylor College of Medicine, Houston, TX
Meeting: 2020 American Transplant Congress
Abstract number: C-186
Keywords: Cytomeglovirus, Pediatric
Session Information
Session Name: Poster Session C: All Infections (Excluding Kidney & Viral Hepatitis)
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Despite widespread use of prevention strategies, CMV remains a common opportunistic infection in SOTR. Contemporary data regarding CMV in pediatric SOTR is limited. We sought to determine the frequency of and risk factors for CMV infection and disease in a large single-center cohort of pediatric SOTR.
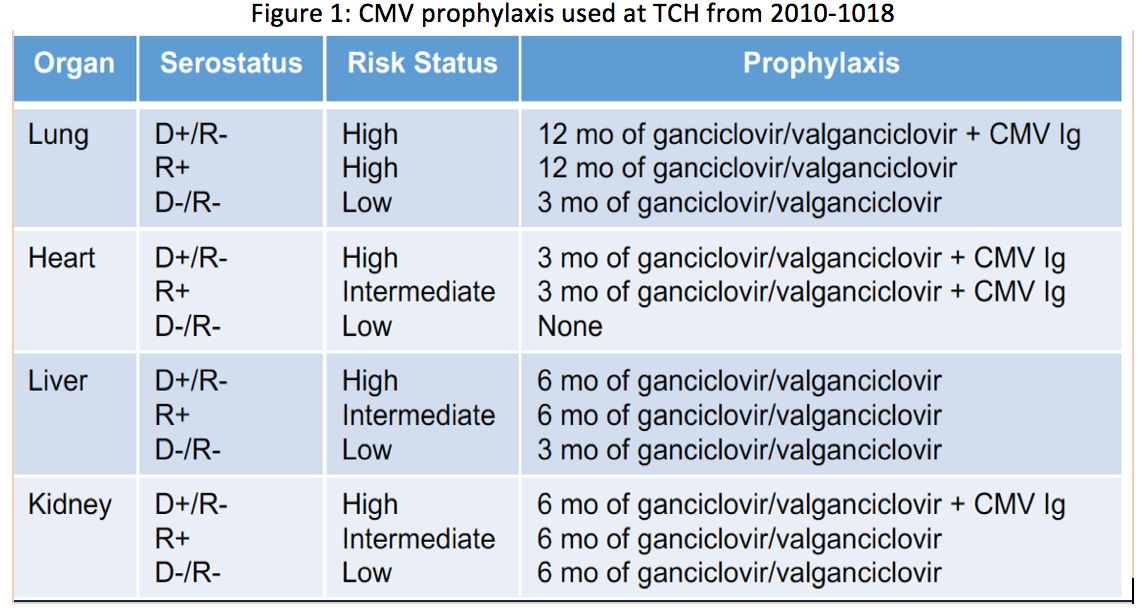
*Methods: A retrospective cohort study of patients < 22 yr of age who received lung, heart, liver, kidney, or multi-organ transplants at TCH between 2010-2018 was completed. Universal CMV prophylaxis was used based on risk status (Figure1). Primary outcome was quantifiable CMV DNAemia. Associations with CMV DNAemia were measured using Fisher exact, Kruskal-Wallis, and multivariate logistic regression. Survival analysis and time to CMV infection were assessed using Kaplan-Meier plots.
*Results: Among 788 SOTR, 132 (17%) had quantifiable CMV DNAemia; this included 20/105 (19%) lung, 69/290 (24%) liver, 28/178 (16%) heart, 2/15 (13%) multi-organ, and 13/200 (7%) kidney recipients. 51 (6%) SOTR had early-onset CMV reactivation while on antiviral prophylaxis. Post-prophylaxis, 59 (7%) SOTR had CMV reactivation and 22 (3%) had primary infection. Median time to quantifiable DNAemia for patients that developed CMV was 290 days post-transplant for lung, 162 for liver, 186 for heart, and 294 for kidney (p<.01), reflecting differences in prophylaxis strategies. High-risk CMV status (D+/R- for heart, liver, kidney and D+ and/or R+ for lung) was associated with CMV DNAemia (p<0.01). Type of organ transplanted also showed an association with CMV DNAemia (p=0.02) with liver transplant recipients more being more likely to have a positive CMV PCR. DNAemia was not associated with age at transplantation, type of organ, or the use of induction immunosuppression. There was no difference in survival during the study follow-up period (1 – 9 yr) for SOTR with vs. without DNAemia (p=0.48).
Overall 22/788 (3%) SOTR had CMV disease, 3 (3%) lung, 4 (2%) heart, 8 (3%) liver, 1 (6%) multi-organ, and 6 (3%) kidney recipients. 20 had CMV syndrome and 2 had tissue invasive disease. Median (range) maximum viral loads were 27700 IU/mL (233-3912694) for SOTR with vs. 900 IU/mL (26-112000) for SOTR without CMV disease (p<0.01).
*Conclusions: This large contemporary cohort of pediatric SOTR on universal prophylaxis demonstrates low overall rates of CMV DNAemia and CMV disease. High-risk CMV status remains associated with CMV DNAemia, suggesting that further interventions targeting this group may be warranted.
To cite this abstract in AMA style:
Valencia K, Hosek K, Moulton E, Munoz F, Demmler-Harrison G, Bocchini C. Epidemiology of Cytomegalovirus (CMV) in Pediatric Solid Organ Transplant Recipients (SOTR) at Texas Children’s Hospital (TCH) [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/epidemiology-of-cytomegalovirus-cmv-in-pediatric-solid-organ-transplant-recipients-sotr-at-texas-childrens-hospital-tch/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress