Elevated Cancer Risk Among US Pediatric Solid Organ Transplant Recipients
1Natl. Cancer Inst., Bethesda, MD
2Seattle Children's Hosp., Seattle, WA
3Cancer Prev. Inst. of CA, Fremont, CA
4U. of Iowa, Iowa City, IA
5NY St. Cancer Reg., Albany, NY
6IL St. Cancer Reg., Springfield, IL
7NJ St. Cancer Reg., Trenton, NJ.
Meeting: 2015 American Transplant Congress
Abstract number: 411
Keywords: Pediatric, Post-transplant lymphoproliferative disorder (PTLD), Post-transplant malignancy
Session Information
Session Name: Concurrent Session: PTLD and Other Malignancies
Session Type: Concurrent Session
Date: Tuesday, May 5, 2015
Session Time: 2:15pm-3:45pm
 Presentation Time: 3:27pm-3:39pm
Presentation Time: 3:27pm-3:39pm
Location: Room 122-AB
Among pediatric transplant recipients, the effects of transplantation and immunosuppression on cancer risk may be unique from those observed in the adult transplant population. No prior study has comprehensively described cancer risk in this population and compared to general pediatric population cancer rates. The US transplant registry was linked to 16 cancer registries to identify cancer diagnoses among solid organ recipients <18 years of age at transplant. Standardized incidence ratios (SIRs) were estimated by dividing observed cancer counts after transplant by expected counts calculated based on general population rates within strata of age, sex, race, calendar year, and registry. We included 17,958 pediatric transplant recipients (44% of the US total). Among these recipients, 394 cancers were diagnosed, 71% of which were non-Hodgkin lymphomas (NHL) and 8% Hodgkin lymphoma (HL). Compared to the general population, cancer incidence was significantly increased overall (SIR=22, 95%CI=20-24) and for NHL, HL, leukemia, myeloma, and cancers of the anus, liver, soft tissue, breast, ovary, vulva, testis, bladder, kidney, and thyroid (Table).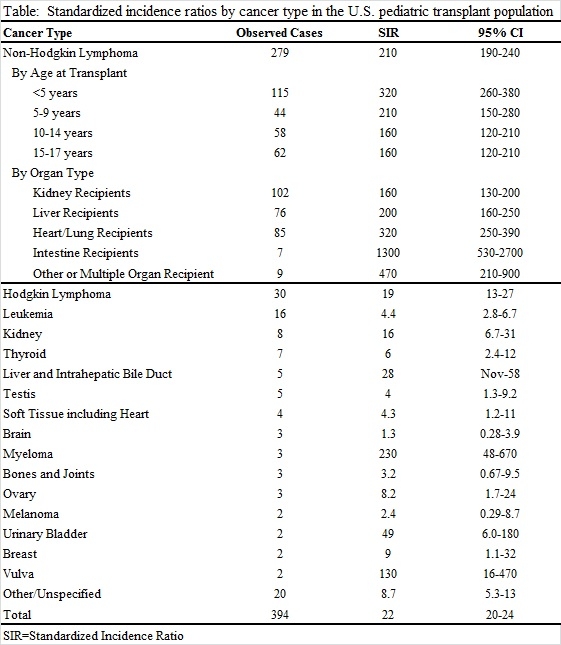 SIRs for lymphomas were highest for recipients <5 years old at transplant (NHL SIR=320, 95%CI=260-380; HL SIR=54, 95%CI=29-92). When evaluated by organ type, NHL risk was most elevated among intestine recipients (SIR=1300, 95%CI=530-2700) followed by heart/lung (SIR=320, 95%CI=250-390), liver (SIR=200, 95%CI=160-250) and kidney recipients (SIR=160, 95%CI=130-200). Pediatric transplant recipients have markedly higher risk for a number of cancers, but the majority of the cancer burden is attributable to NHL. Increased NHL risk was exceedingly high among the youngest recipients, who are likely to develop primary Epstein-Barr virus infection after transplantation, and among intestine recipients.
SIRs for lymphomas were highest for recipients <5 years old at transplant (NHL SIR=320, 95%CI=260-380; HL SIR=54, 95%CI=29-92). When evaluated by organ type, NHL risk was most elevated among intestine recipients (SIR=1300, 95%CI=530-2700) followed by heart/lung (SIR=320, 95%CI=250-390), liver (SIR=200, 95%CI=160-250) and kidney recipients (SIR=160, 95%CI=130-200). Pediatric transplant recipients have markedly higher risk for a number of cancers, but the majority of the cancer burden is attributable to NHL. Increased NHL risk was exceedingly high among the youngest recipients, who are likely to develop primary Epstein-Barr virus infection after transplantation, and among intestine recipients.
To cite this abstract in AMA style:
Yanik E, Smith J, Shiels M, Clarke C, Lynch C, Kahn A, Koch L, Pawlish K, Engels E. Elevated Cancer Risk Among US Pediatric Solid Organ Transplant Recipients [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/elevated-cancer-risk-among-us-pediatric-solid-organ-transplant-recipients/. Accessed February 20, 2026.« Back to 2015 American Transplant Congress
