Effects of New KPD Histocompatibility Policy on Refusal Rate and Transplants.
1UNOS, Richmond, VA
2Univ Hosp Med Ctr, Cleveland, OH
3Johns Hopkins Univ, Baltimore, MD
4SW Immunodiagnostics, San Antonio, TX
5Cedars-Sinai Health, Los Angeles, CA
6Mass Gen Hosp, Boston, MA
7Carnegie Mellon Univ, Pittsburgh, PA
8Emory Univ, Atlanta, GA
Meeting: 2017 American Transplant Congress
Abstract number: 334
Keywords: Histocompatibility, HLA matching, Kidney, Kidney transplantation
Session Information
Session Name: Concurrent Session: Health Services and Policy in Organ Transplanation
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: E271a
Background: Transplant centers commonly refuse kidney paired donation (KPD) match offers due to unacceptable crossmatch (XM). To reduce XM refusals a new OPTN KPD histocompatibility policy requiring reporting of all donor antigens, periodic retesting of candidate unacceptables, and specific screening requirements was implemented on 1/21/16.
Methods: XM refusal rates were compared for pre (6/2/14–1/21/16) vs post (1/22/16–9/26/16) policy periods. A logistic regression model analyzed match outcomes of transplanted or not transplanted controlling for the time periods, candidate CPRA, candidate age, donor age, donor BMI, and donor ABO.
Results: XM related refusal rate decreased from 29% (n=1063) pre to 11% (n=262) post policy implementation with a greater decrease in virtual (21% vs 6%) vs physical (8% vs 5%) XM refusals. The policy also significantly increased the log odds of a match proceeding to transplant (0.76, p=0.002). Figure 1 compares the modeled predicted probability of transplant between the periods for CPRA (A), donor BMI (B), and donor age (C). With the exception of the x-axis variable, the other variables are held constant at data set means.
Conclusions: The new KPD histocompatibility policy demonstrated a decline in KPD XM refusal rate while increasing the probability of transplant. Many highly sensitized candidates became ineligible for match runs immediately after implementation and the mean CPRA of matched candidates decreased. The mean CPRA of eligible candidates, however, is now increasing as unacceptables are updated. Longer term analysis will determine whether the increased probability of transplant resulted from the policy's intention vs ineligibility of some sensitized candidates. Further improvements to the program will be based on longer term findings.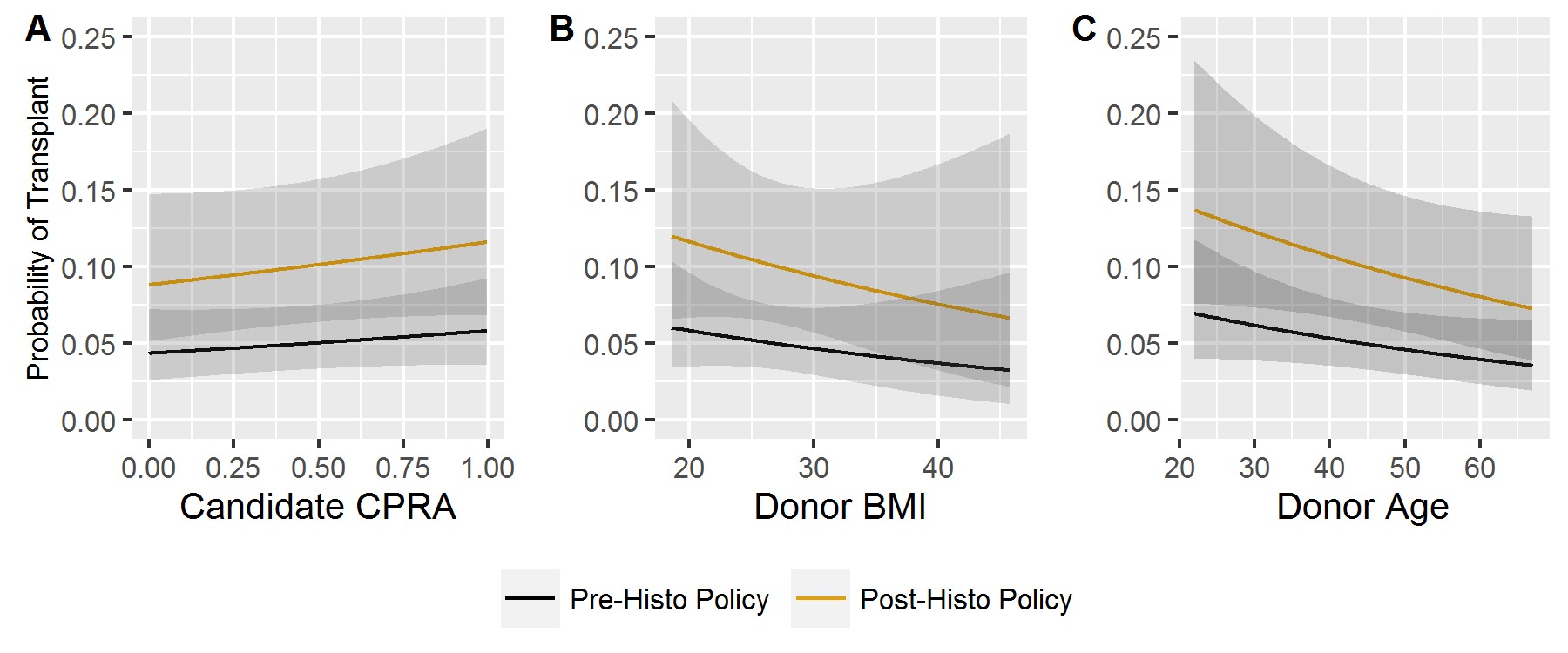
CITATION INFORMATION: Leishman R, Aeder M, Leffell M, Murphey C, Reinsmoen N, Saidman S, Sandholm T, Toll A, Harper A, Turgeon N. Effects of New KPD Histocompatibility Policy on Refusal Rate and Transplants. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Leishman R, Aeder M, Leffell M, Murphey C, Reinsmoen N, Saidman S, Sandholm T, Toll A, Harper A, Turgeon N. Effects of New KPD Histocompatibility Policy on Refusal Rate and Transplants. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/effects-of-new-kpd-histocompatibility-policy-on-refusal-rate-and-transplants/. Accessed March 4, 2026.« Back to 2017 American Transplant Congress
