Economic and Clinical Consequences of ABO Incompatible Kidney Transplantation: A National Database Study, The
Dartmouth Univ
Saint Louis Univ
Johns Hopkins Univ
Washington Univ
Meeting: 2013 American Transplant Congress
Abstract number: 483
ABO incompatible (ABOi) live donor kidney transplantation (LKDT) accompanied by plasmapheresis can offer a transplant option superior to continued waiting on dialysis. However, further expansion of ABOi transplantation has been constrained by economic considerations despite the lack of robust cost data. The United States Renal Data System registry data for Medicare-insured LDKT recipients in 2000-2007 (n=13,500) were analyzed to assess the economic and survival outcomes of ABOi LKDT in a nationally representative cohort.
ABOi (n=124) LDKTs were identified using donor and recipient ABO group as reported to the national registry. A2-to-O (A2O, n =30) LDKTs were categorized separately, due to increasing data that A2O transplantation may be safe without additional treatment. Patient and graft survival were assessed with Cox regression, while variation in costs, defined as total Medicare payments in periods of interest, was compared using multivariate linear regression. Covariates included recipient, donor and transplant factors in the UNOS Kidney Allocation Review Committee survival model. Post-transplant cost samples were limited to patients with continuous Medicare coverage, graft loss or death during a period.
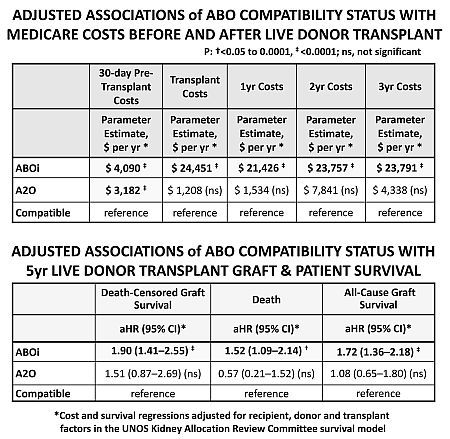
Recipients of ABOi ($4,090) and A2O ($3,182) LDKTs experienced increased adjusted costs in the 30 days pre-transplant (Table 1). Compared with compatible LDKT, ABOi was also associated with $24,451 increased costs at transplant, as well as persistent increases of $21,500 to $23,800 in years 1, 2 and 3 (Table 1). The A2O group did not experience higher transplant or later costs. ABOi transplants had a 72% higher relative risk of 5yr all-cause graft loss, while A2O did not have significant survival implications (Table 2).
ABOi offers patients with potential living donors an additional option for transplantation. While more expensive than compatible transplants, the costs are significantly lower than long-term dialysis. The etiology of the increased costs beyond the transplant episode requires further analyses.
To cite this abstract in AMA style:
Simpkins C, Lentine K, Xiao H, Schnitzler M, Tuttle-Newhall J, Segev D, Dharnidharka V, Brennan D, Axelrod D. Economic and Clinical Consequences of ABO Incompatible Kidney Transplantation: A National Database Study, The [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/economic-and-clinical-consequences-of-abo-incompatible-kidney-transplantation-a-national-database-study-the/. Accessed July 18, 2025.« Back to 2013 American Transplant Congress
