Early Steroid Withdrawal in African American Kidney Transplant Recipients: A Propensity Score Matching Analysis.
MUSC, Charleston, SC.
Meeting: 2016 American Transplant Congress
Abstract number: 286
Keywords: African-American, Immunosuppression, Kidney transplantation, Safety
Session Information
Session Name: Concurrent Session: Belatacept and Steroid Withdrawal in Kidney Transplantation
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: Ballroom A
Objective: The aim of this study was to assess the safety of steroid withdrawal in African American (AA) kidney transplant (KTX) recipients.
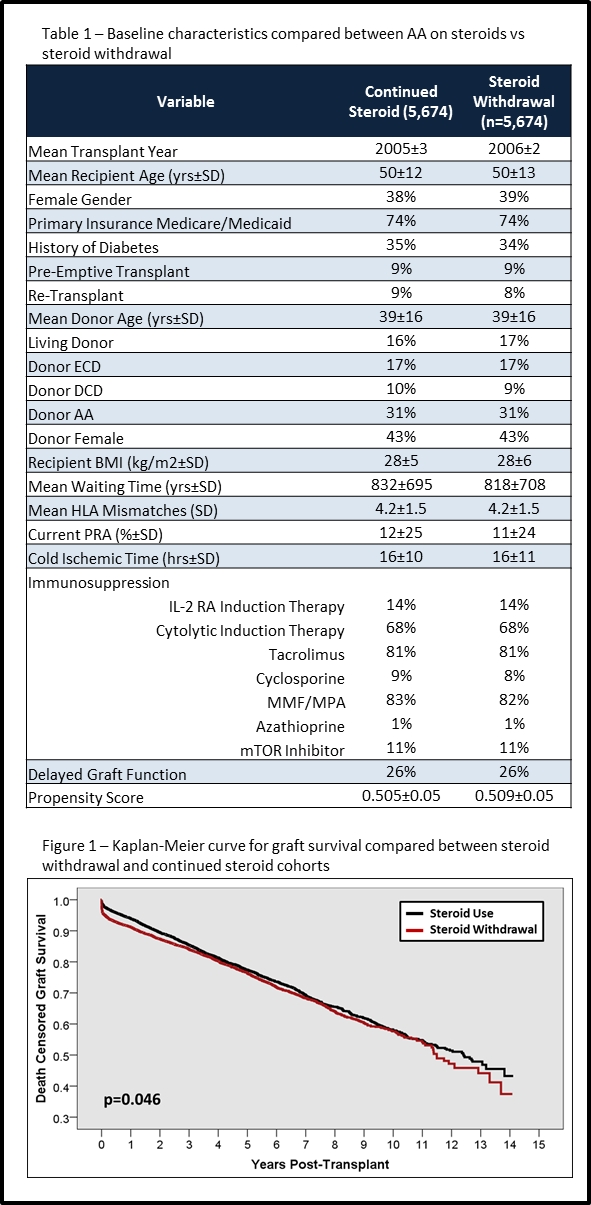
Methods: Longitudinal cohort study using national UNOS registry data and propensity score matching (PSM), including all adult AA KTX transplanted between 2000 and 2009. PSM was used to equalize risk across steroid use (SU) and steroid withdrawal (SW) groups based on all the variables in Table 1.
Results: Of 34,357 AA KTX, 5,674 (16.5%) had SW; the SW was matched 1:1 to 5,674 SU AAs. The PSM produced two cohorts that were exceptionally similar at baseline for known risks and confounders (Table 1). Outcome analysis revealed that acute rejection rates were higher in the SU group (13.1% vs 10.9%, p<0.001), while overall and death censored graft loss rates were marginally lower in the SW group (Figure 1, p<0.05). The impact of SW on graft loss was significantly modified by cytolytic induction (ORno cyto 1.25 vs 0.83), tacrolimus (ORno tac 1.29 vs 0.88), MMF/MPA (ORno MMF 1.15 vs 0.91) and DGF (ORDGF 1.27 vs 0.85), but not rejection (ORrej 1.0 vs 0.98). Creatinine at last follow up was slightly higher in the SW cohort (median [IQR] 2.6 [1.6,5.3] vs 2.7 [1.6-5.7] mg/dL; p=0.016).
Conclusions: Steroid withdrawal in AA KTX recipients appears to marginally increase the risk of graft loss, which is independent of acute rejection. Use of potent immunosuppression (cytolytic induction with tac/MMF or tac/mTOR) likely mitigates this risk, except in those that develop delayed graft function.
CITATION INFORMATION: Taber D, Gebregziabher M, Srinivas T, Chavin K, Baliga P, Egede L. Early Steroid Withdrawal in African American Kidney Transplant Recipients: A Propensity Score Matching Analysis. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Taber D, Gebregziabher M, Srinivas T, Chavin K, Baliga P, Egede L. Early Steroid Withdrawal in African American Kidney Transplant Recipients: A Propensity Score Matching Analysis. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/early-steroid-withdrawal-in-african-american-kidney-transplant-recipients-a-propensity-score-matching-analysis/. Accessed July 12, 2025.« Back to 2016 American Transplant Congress
