Early Prediction of Human Renal Allograft Rejection (AR) by Inflammatory Transitional B Cells
1Starzl Transplantation Institute, UPMC, Pittsburgh, PA, 2UCL, London, United Kingdom
Meeting: 2020 American Transplant Congress
Abstract number: 306
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes III
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: Early prediction of AR within the 1st post-transplant year could identify at-risk patients for targeted therapeutic interventions to mitigate risk and improve outcomes.
*Methods: In this prospective, multicenter observational study, we examined human B cells and their cytokines to perform as a biomarker for AR. PBMCs were stimulated (CpG+CD40L X 24h) and B cell subsets examined for IL10 and TNFα expression by flowcytometry.
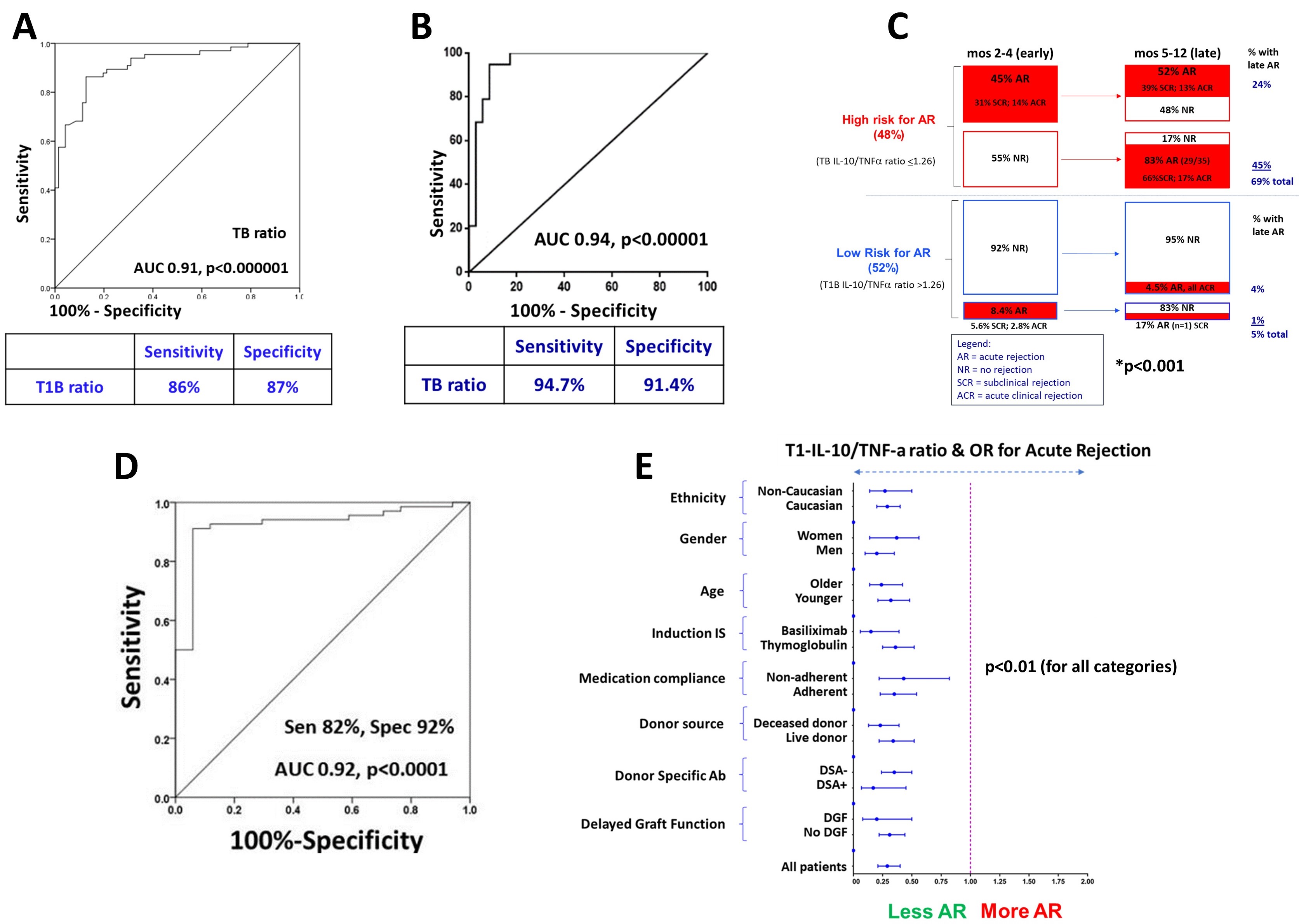
*Results: 165 patients transplanted between years 2013-14 consented to participate in the training set. Blood was drawn at 0,1,3,6 &12mos to examine B cells and DSA. Patients underwent 2 protocol biopsies (bx) along with any for-cause bx. Baseline features of the study patients were comparable to those who did not consent to participate. A low IL10/TNFα ratio within transitional B cells (TBs) at 3mo predicted AR within the 1st yr (Fig1A). These results were validated in a further prospective cohort of 90 patients transplanted in 2015 (Fig 1B). When the progression of AR was examined with serial biopsies in patients with low cytokine ratio, 83% with no early AR (0-6mos) developed late AR (6m-1y), while a remarkable 52% had recurrent/recalcitrant AR despite therapy. On the contrary, very few patients with high cytokine ratio either had early, late or recurrent rejection (Fig 1C). Cytokine ratio for the prediction of AR was further validated in an external cohort of 90 patients (Fig 1D). In a stratified analysis, a low cytokine ratio was strongly associated with AR in distinct patient sub-groups defined by age, gender, race, IS, DSA, DGF and therapy adherence (Fig 1E). There was no difference in the cytokine ratio between TCMR and ABMR. Finally, TB cytokine ratio was significantly lower in patients with DSA and more importantly, predicted AR in such patients. Thus, B cells in high-risk patients are polarized towards a pro-inflammatory cytokine profile. Culture of such B cells with α-TNF, reversed this polarization profile. Such reversal was noted in all the B subsets, although pronounced in the TBs. TNF blocked B cells suppressed autologous T cell TNFα while increasing IL10 expression. Thus, α-TNF restored Breg activity in high-risk patients. Finally, α-TNF inhibited in vitro differentiation of B cells to plasma cells while increasing their IL-10. There was a selective depletion of complement fixing IgG subclasses in their culture supernatants.
*Conclusions: Thus, we tested and validated the use of TB cytokines to predict AR and provided an ex vivo rationale for possible therapeutic intervention with TNF blockade.
To cite this abstract in AMA style:
Cherukuri A, Sharma A, Mehta R, Sundaram H, Salama A, Rothstein D. Early Prediction of Human Renal Allograft Rejection (AR) by Inflammatory Transitional B Cells [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/early-prediction-of-human-renal-allograft-rejection-ar-by-inflammatory-transitional-b-cells/. Accessed March 3, 2026.« Back to 2020 American Transplant Congress