Early Outcome of Heart-Kidney Transplantation in the Current Heart Allocation System in the United States
1University of Virginia, Charlottesville, VA, 2Johns Hopkins Medical Institute, Baltimore, MD, 3Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Meeting: 2021 American Transplant Congress
Abstract number: 413
Keywords: Bioequivalence, Heart/lung transplantation, Kidney transplantation, Outcome
Topic: Clinical Science » Public Policy » Non-Organ Specific: Public Policy & Allocation
Session Information
Session Name: Adherence, Economics, and Ethics
Session Type: Poster Video Chat
Date: Sunday, June 6, 2021
Session Time: 7:30pm-8:30pm
 Presentation Time: 7:30pm-7:40pm
Presentation Time: 7:30pm-7:40pm
Location: Virtual
*Purpose: In the United States, heart allograft allocation is a primary determinant for heart-kidney transplantation (HKT). We analyzed the OPTN dataset and compared the outcomes of HKT performed under the prior heart allocation system (prior-HAS, October 1, 2015-October 18, 2018, n= 516) and the current-HAS which prioritized sicker patients (after October 18, 2018, n=149)).
*Methods: We acquired de-identified data from the OPTN registry with follow up through December 6, 2019.Baseline demographics, comorbidities, etiology of cardiac and kidney dysfunction were collected. Pre-transplant cardiac support was assessed by inotropic and/or mechanical circulatory support (MCS). The kidney dysfunction pre-transplant was assessed by the serum creatinine at listing, the need for pre-transplant dialysis, and duration of dialysis (short ≤6 weeks, medium 7-12, long >12 weeks).
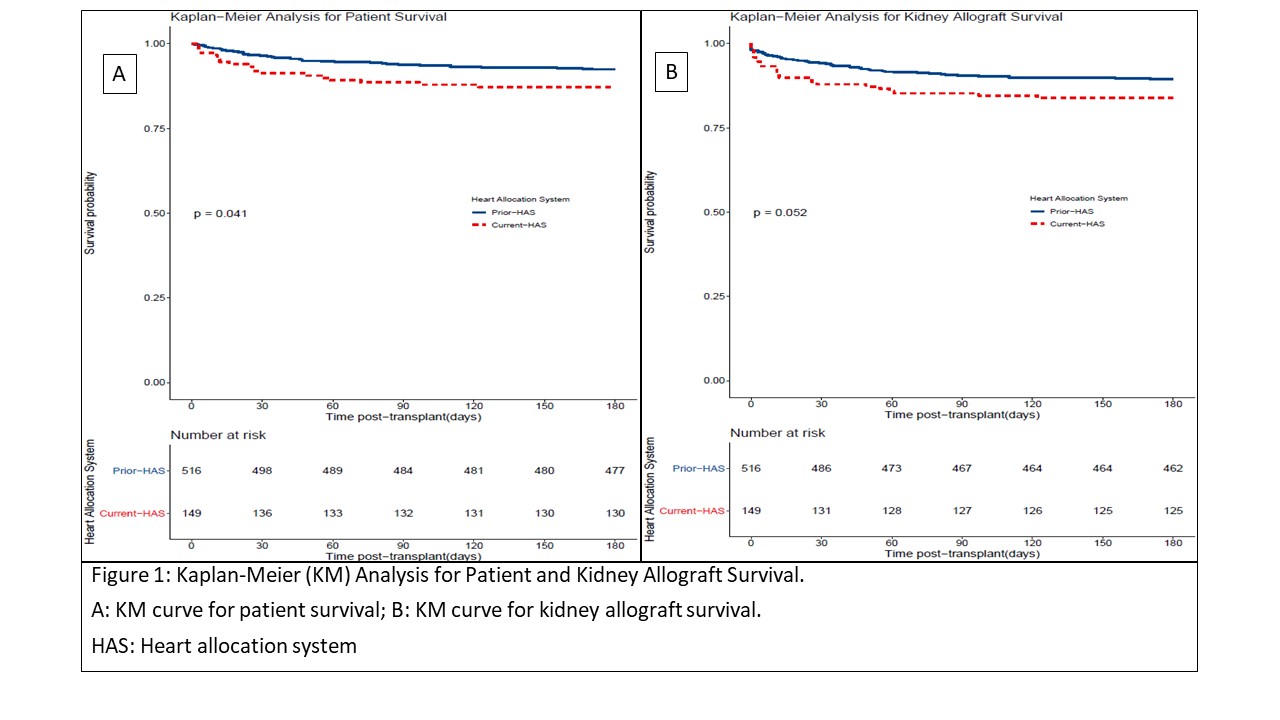
*Results: Under the current-HAS, the percentage of HKT amongst the total heart transplants has increased to 6.4% from 5.3% (p=0.038). Although the prevalence of pre-transplant dialysis was similar (about 50%) amongst the groups, a higher percentage in the current-HAS group had a short duration (less than 6 weeks) of dialysis (24.5% vs 7.3%, p= 0.01). On univariate Cox-regression, the current-HAS group had lower 180-day survival (87.2% vs 92.4%, HR 1.75, 95%CI 1.01-3.04, p=0.04) and a trend towards lower kidney allograft survival (83.9% vs 85.9%, HR 1.60, 95%CI 0.09-2.59, p= 0.05). After adjusting for covariates, HAS era was not an independent predictors of outcomes. Delayed graft function of kidney allograft remained a strong predictor of poorer outcomes and was higher in the current-HAS group (35% vs 26%, p=0.03).
*Conclusions: Our study shows that the rates of HKT have continued to increase under the current HAS. Similar to the higher mortality in heart transplant recipients under the current-HAS era, patient mortality was higher in the HKT recipients too. This study highlights the need for a novel HKT allocation policy with standardized listing and allocation criteria aimed to improve HKT outcomes.
To cite this abstract in AMA style:
Rao S, Doyle A, Brennan D, Constantinescu S. Early Outcome of Heart-Kidney Transplantation in the Current Heart Allocation System in the United States [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/early-outcome-of-heart-kidney-transplantation-in-the-current-heart-allocation-system-in-the-united-states/. Accessed March 3, 2026.« Back to 2021 American Transplant Congress