Early Hospital Readmission Among Immunologically Vulnerable Kidney Transplantation Recipients.
Surgery, Johns Hopkins University, School of Medicine, Baltimore, MD.
Meeting: 2016 American Transplant Congress
Abstract number: A102
Keywords: High-risk, Kidney transplantation, Outcome
Session Information
Session Name: Poster Session A: Kidney Desensitization
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
BACKGROUND: We previously established that 31% of all kidney transplant (KT) recipients experience early hospital readmission (EHR), or readmission within 30 days of discharge following KT. While HLA-incompatible (HLAi) and ABO-incompatible (ABOi) KT recipients require more extensive post-transplant protocols, the incidence of EHR is unknown.
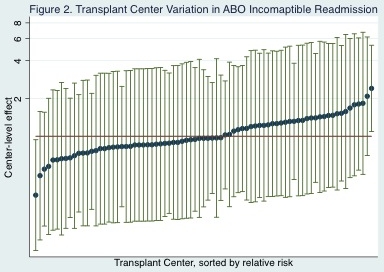
METHODS: We used USRDS data and medical records data from 17 centers performing IKT to study 248 adult Medicare primary HLAi recipients, and USRDS data to study 258 adult Medicare primary ABOi recipients. We matched each IKT and ABOi recipient with compatible live donor KT recipients, using iterative radius matching (1:5), matched on age, blood type, PRA, renal replacement time, prior transplant, sex, diabetes, and year. The incidence of EHR was compared between incompatible recipients and matched controls, accounting for clustering among controls. Empirical Bayes estimation was used to determine variation in EHR across transplant centers.
RESULTS: IKT recipients had a 62.1% incidence of EHR compared with 56.3% in their matched counterparts, a finding that approached statistical significance (p=0.09). ABOi recipients had a 37.3% incidence of EHR compared with 31.5% in their matched counterparts, a finding that approached statistical significance (p=0.07). There was almost no variation in the rate of EHR for HLAi or ABOi recipients across centers.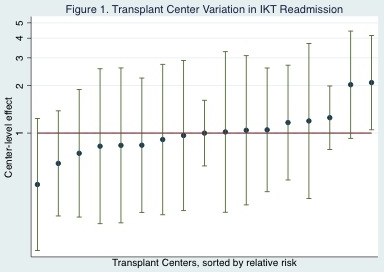
CONCLUSIONS: The incidence of EHR among HLAi recipients is substantially higher than the published incidence for all KT recipients, while the incidence of EHR is minimally higher among ABOi recipients. Compared to matched controls, there is no statistically significant difference in the incidence of EHR for HLAi or ABOi recipients. High EHR may be related to the type of patients that require HLAi or ABOi rather than the transplant itself.
CITATION INFORMATION: King E, Orandi B, Bae S, Luo X, Segev D. Early Hospital Readmission Among Immunologically Vulnerable Kidney Transplantation Recipients. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
King E, Orandi B, Bae S, Luo X, Segev D. Early Hospital Readmission Among Immunologically Vulnerable Kidney Transplantation Recipients. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/early-hospital-readmission-among-immunologically-vulnerable-kidney-transplantation-recipients/. Accessed July 14, 2025.« Back to 2016 American Transplant Congress
