Early Clinical Complications Following HLA-Incompatible Living Donor Kidney Transplantation
1Johns Hopkins University, Baltimore, MD, 2University of Wisconsin-Madison, Madison, WI
Meeting: 2022 American Transplant Congress
Abstract number: 400
Keywords: HLA antibodies, Kidney, Post-operative complications, Surgical complications
Topic: Clinical Science » Kidney » 36 - Kidney Immunosuppression: Desensitization
Session Information
Session Name: Kidney Immunosuppression: Desensitization & Acute Antibody Mediated Rejection
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 3:30pm-3:40pm
Presentation Time: 3:30pm-3:40pm
Location: Hynes Ballroom A
*Purpose: Incompatible living donor kidney transplant recipients (ILDKTr) require desensitization to facilitate transplantation across donor-specific antibody (DSA); however, this substantial upfront immunosuppression may result in higher risk of early complications following surgery.
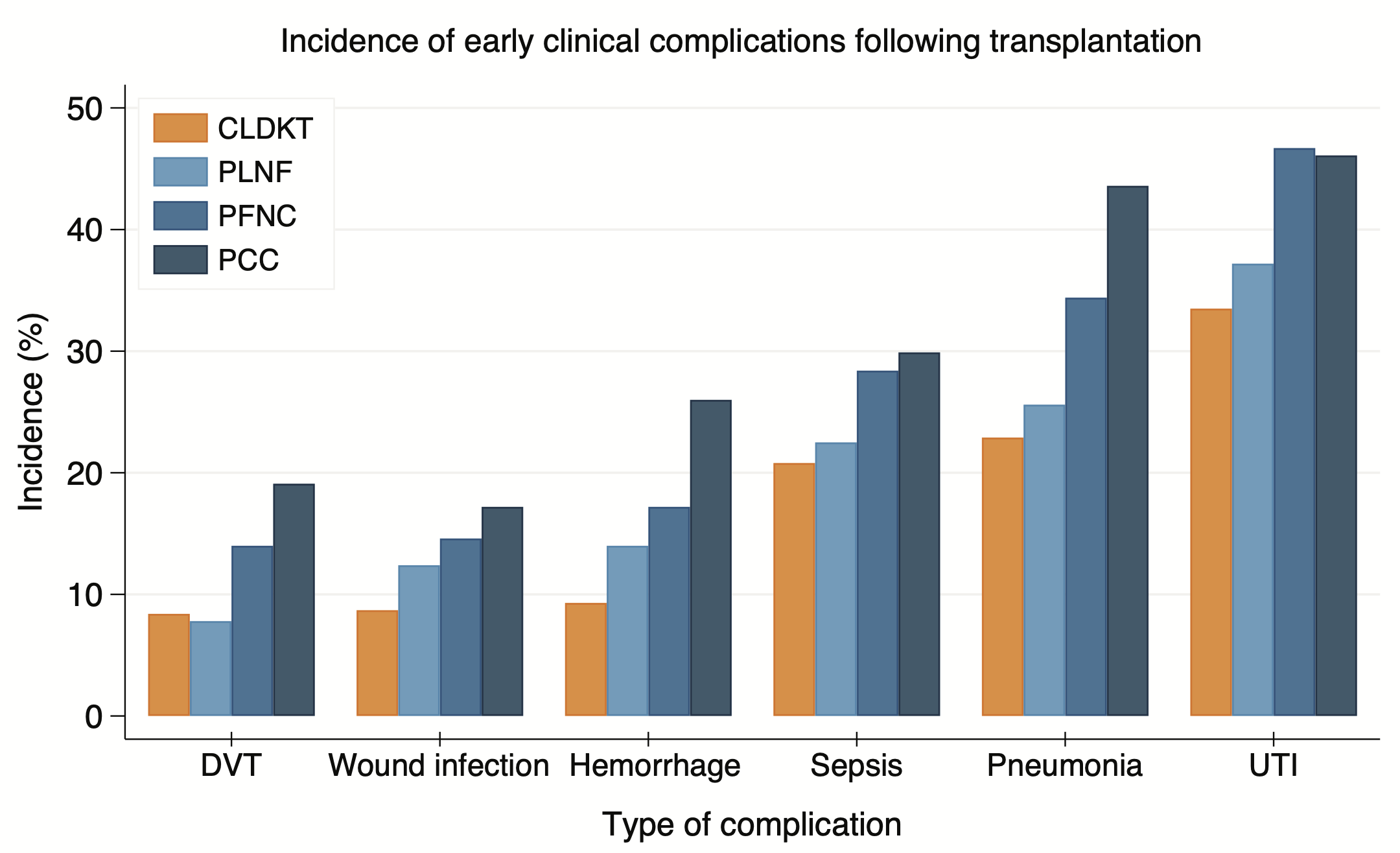
*Methods: We compared 682 ILDKT to 5685 compatible LDKT (CLDKTr) Medicare-primary recipients drawn from a 25-center cohort with novel linkage to the United States Renal Data System from 1999-2014. We characterized DSA strength as positive-Luminex, negative-flow crossmatch (PLNF, n=129); positive-flow, negative-cytotoxic crossmatch (PFNC, n=349); or positive-cytotoxic crossmatch (PCC, n=204). Diagnoses of deep vein thrombosis (DVT), wound infection, hemorrhage, sepsis, pneumonia, and urinary tract infection (UTI) were ascertained using ICD-9 codes. We used weighted by the odds Cox regression models to quantify the risk of early complications in the first three months, and from three months to one-year post-transplant.
*Results: Compared to CLDKTr, ILDKTr had higher incidence of DVT (14.4% vs. 8.4%), wound infection (15.0% vs. 8.7%), hemorrhage (19.2% vs. 9.3%), sepsis (27.7% vs 20.8%), pneumonia (35.5% vs. 22.9%), and UTI (44.7% vs. 33.5%) (p for all comparisons<0.001) (Figure 1). Within the first three months, a higher risk of DVT (wHR PLNF=0.050.453.93;PFNC=0.941.793.39;PCC=1.001.883.52), wound infection (wHR PLNF=0.691.232.19;PFNC=1.241.602.06;PCC=0.801.693.62), and hemorrhage (PLNF=1.111.963.47;PFNC=0.911.823.65;PCC=2.072.964.21) were observed across varying levels of DSA strength; however, the risk of these complications decreased thereafter. Although there was no evidence of increased risk of sepsis with the first three months, this risk subsequently increased (wHR PLNF=0.811.874.28;PFNC=0.991.502.30;PCC=1.102.314.81). In contrast, there was higher risk of pneumonia that persisted throughout both time periods (0-3 months wHR PLNF=0.851.914.29; PFNC=1.142.073.75;PCC=1.342.735.59; >3 months wHR PLNF=1.241.571.99;PFNC=0.811.422.49;PCC=1.051.913.48).
*Conclusions: Providers should consider these risks during pre-operative counselling, and awareness may aid to improve protocols for ILDKT patient management.
To cite this abstract in AMA style:
Motter JD, Jackson K, Massie A, Garonzik-Wang J, Segev D. Early Clinical Complications Following HLA-Incompatible Living Donor Kidney Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/early-clinical-complications-following-hla-incompatible-living-donor-kidney-transplantation/. Accessed February 24, 2026.« Back to 2022 American Transplant Congress