Duration of Pre-Transplant Abstinence Does Not Predict Severe Relapses of Alcohol Abuse in High-Risk Alcoholic Liver Transplant Recipients
Emory Transplant Center, Atlanta, GA
Meeting: 2020 American Transplant Congress
Abstract number: C-165
Keywords: Alcohol, Liver transplantation
Session Information
Session Name: Poster Session C: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The traditional requirement of >6 months pre-transplant sobriety for liver transplant recipients has been challenged by emerging literature, but risk factors for post-transplant recidivism and poor transplant outcomes in high-risk alcoholic recipients remain ill-defined.
*Methods: We performed one of the largest contemporary retrospective case series of patients transplanted for alcoholic liver disease, identifying 270 patients transplanted at Emory University between 1/1/2013 and 4/15/2019. This date range was chosen to highlight recent changes in nationwide transplant practices after the publication of literature supportive of transplanting alcoholics with <6 months of pre-transplant sobriety. Patient records were examined for pre-transplant risk factors (e.g. duration of pre-transplant sobriety, DUI history, age/gender, drug use and rehab history) and subsequent post-transplant alcohol use (documented by history or urine ethyl glucuronide). Evidence of allograft injury or alcohol-related complication were used to categorize relapses as mild or severe.
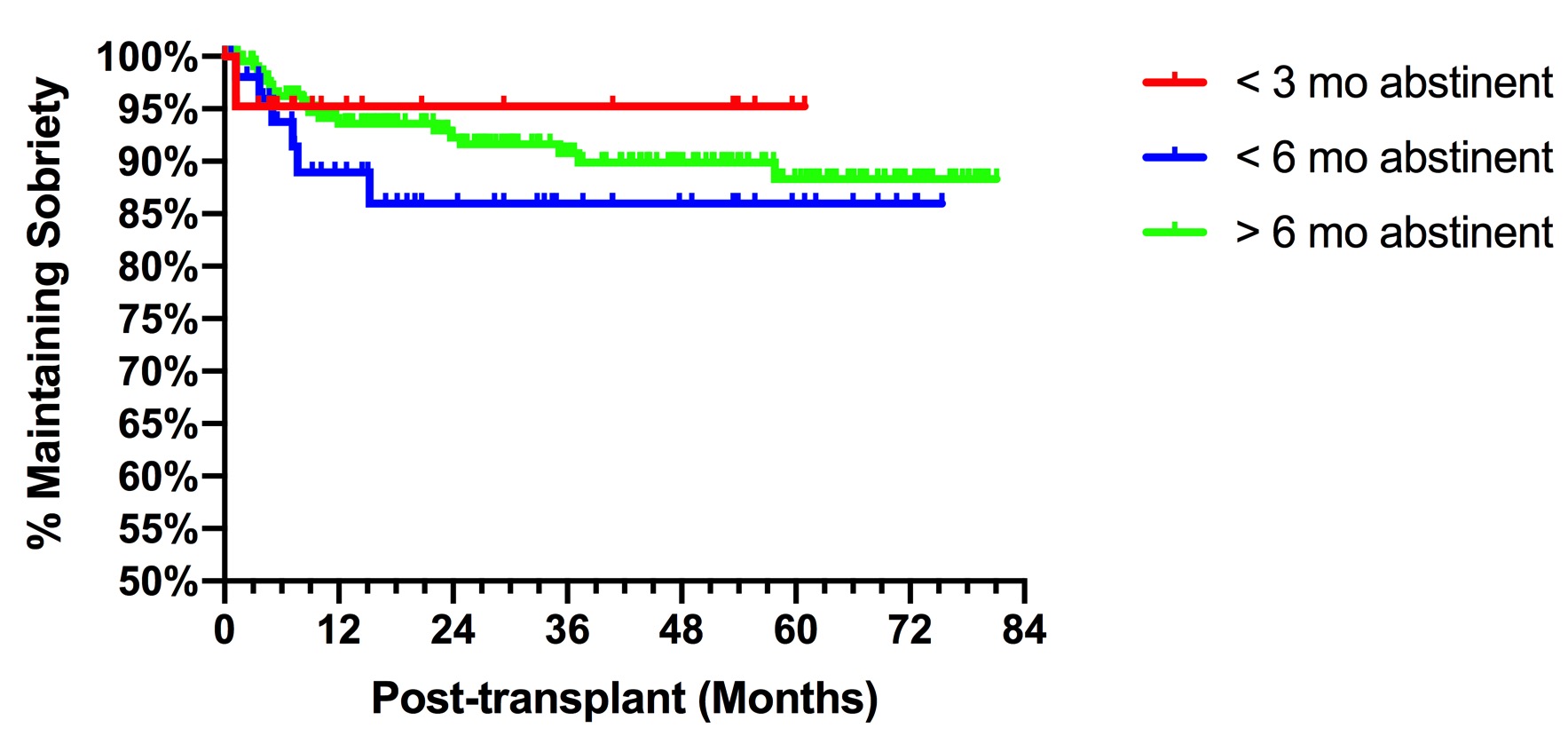
*Results: Over these years, the incidence of high-risk alcoholics with <3 months pre-transplant sobriety increased from 0% to 21.4% of alcoholics transplanted (p=0.0003). Compared to patients with >6 months pre-transplant sobriety, those with <3 months had higher MELD at transplant (37.7 vs. 29.3, p=0.0001) and were more likely hospitalized in the ICU (60.9% vs. 19.4%, p=0.001). Of the total cohort, 14% demonstrated some post-transplant alcohol use and over half of these patients (64.1%) experienced severe relapse with evidence of allograft injury. Risk factors for any post-transplant recidivism include recent DUI (OR 7.09, 95% CI:2.16-23.28), age <45 years-old (OR 3.48, CI:1.69-7.17), female gender (OR 3.05, CI:1.52-6.11), history of rehab/AA (OR 2.42, CI:1.22-4.81) and <6 months pre-transplant sobriety (OR 2.50, CI:1.18-5.28). Kaplan-Meier analysis demonstrated equivalent survival in recipients with <3 months and >6 months sobriety. Importantly, although recipients with <6 months pre-transplant sobriety had higher rates of any alcohol use post-transplant, the risk of allograft-injuring severe relapse was not impacted by either <3 month or <6 month duration of pre-transplant sobriety (OR 1.39, CI:0.53-3.67).
*Conclusions: This study suggests that carefully selected high-risk alcoholics with <3 months pre-transplant sobriety can undergo liver transplantation with acceptable post-transplant outcomes and recidivism risks. Other risk factors (e.g. recent DUI and young age) may be more predictive of severe relapse.
To cite this abstract in AMA style:
Kitchens WH. Duration of Pre-Transplant Abstinence Does Not Predict Severe Relapses of Alcohol Abuse in High-Risk Alcoholic Liver Transplant Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/duration-of-pre-transplant-abstinence-does-not-predict-severe-relapses-of-alcohol-abuse-in-high-risk-alcoholic-liver-transplant-recipients/. Accessed March 4, 2026.« Back to 2020 American Transplant Congress