Donor Recipient Matching Based on HLA Epitopes Improves Outcome in Kidney Transplant Recipients.
1Nephrology, Charité
Universitaetsmedizin, Berlin, Germany
2HLA Laboratory, Charité
Universitaetsmedizin, Berlin, Germany
3PIRCHE, Berlin, Germany
4Laboratory of Translational Immunology, UMC Utrecht, Utrecht, Netherlands
Meeting: 2017 American Transplant Congress
Abstract number: 432
Keywords: Allocation, Epitopes, Graft survival, Outcome
Session Information
Session Name: Concurrent Session: Kidney Optimizing Donor/Recipient Selection and Matching
Session Type: Concurrent Session
Date: Tuesday, May 2, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: E450a
Background: HLA mismatches of the donor and recipient causing de novo donor-specific HLA antibodies (dnDSA) are a risk factor for immunologic complications and poor graft survival. Evaluating histocompatibility based on HLA epitopes may improve outcomes after kidney transplantation and better prevent sensitization than classical matching of HLA class I and II antigens. To date there is very few data examining clinical outcomes based on HLA epitope matching.
Patients and methods: 2,787 consecutive adult kidney transplants performed 1995-2015 without preformed DSA have been included. De novo DSA were detected by Luminex single antigen assay. HLAMatchmaker score was calculated as the weighted sum of eplets of high resolution patient and donor typing.
Results: The distribution of the HLA epitope mismatch (assessed by the HLAMatchmaker algorithm) and the correlation to the count of mismatched A,B,C,DR,DQ-HLA molecules is shown in Fig.1a and Fig.1b. Categorization by HLAMatchmaker epitopes significantly predicted the incidence of dnDSA (Fig.1c) and allograft survival (Fig.1d). In a multivariate Cox regression analysis adjusted for the number of antigen mismatches the HLAMatchmaker score could be identified as an independent risk factor for dnDSA (HR per 10 increment 1.269 (p<0.0001) adjusted for A,B,DR-antigen mismatches; HR 1.270 (p<0.0001) per 10 increment adjusted for A,B,C,DR,DQ-antigen mismatches).
Conclusions: HLAMatchmaker epitopes have a strong predictive value for dnDSA independently from the antigen mismatch. Allocation strategies based on HLA epitopes may result in improved donor recipient matching with a smaller amount of immunogenicity leading to less dnDSA and thus improve long-term kidney allograft survival.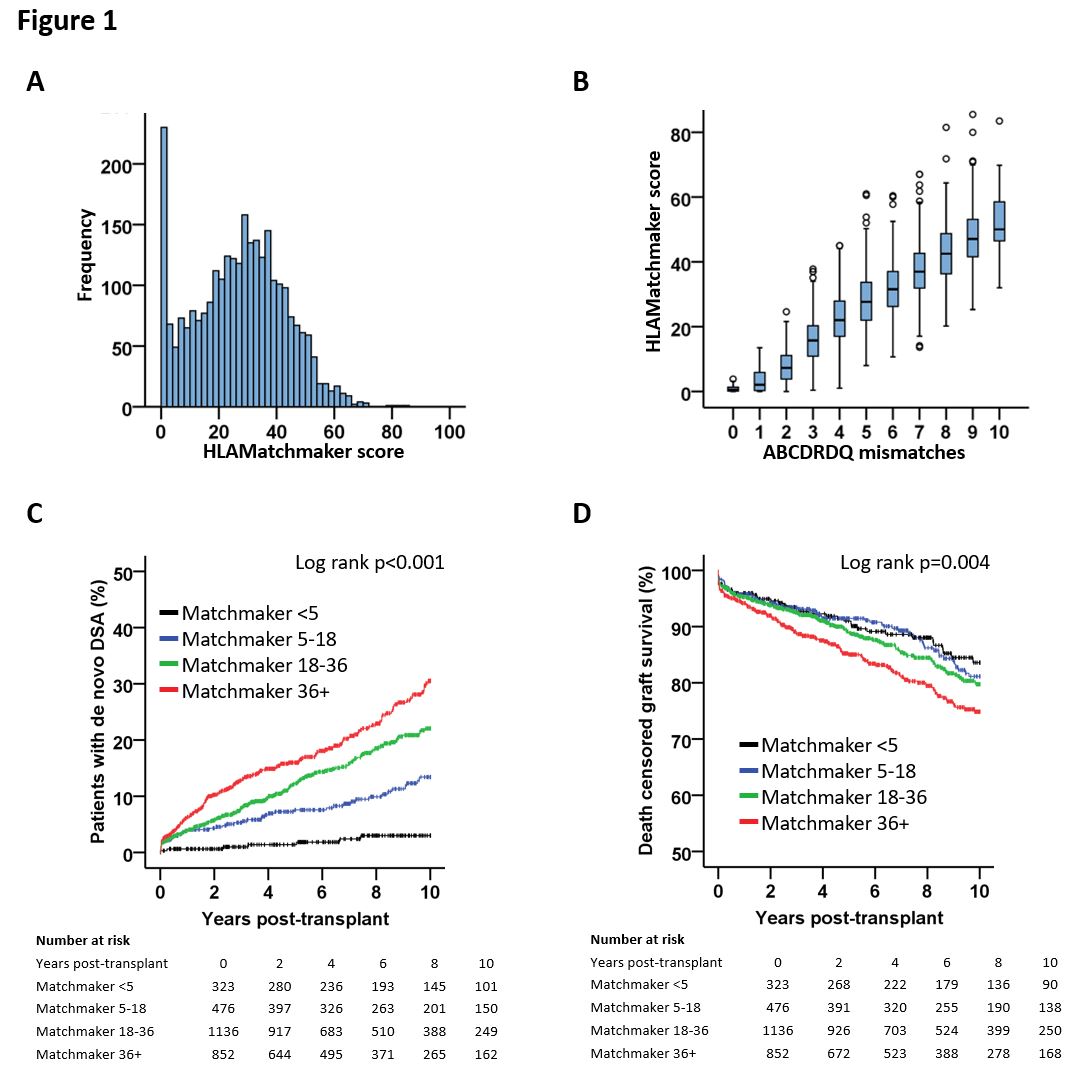
CITATION INFORMATION: Staeck O, Niemann M, Halleck F, Khadzhynov D, Schönemann C, Reinke P, Spierings E, Budde K, Lachmann N. Donor Recipient Matching Based on HLA Epitopes Improves Outcome in Kidney Transplant Recipients. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Staeck O, Niemann M, Halleck F, Khadzhynov D, Schönemann C, Reinke P, Spierings E, Budde K, Lachmann N. Donor Recipient Matching Based on HLA Epitopes Improves Outcome in Kidney Transplant Recipients. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/donor-recipient-matching-based-on-hla-epitopes-improves-outcome-in-kidney-transplant-recipients/. Accessed March 4, 2026.« Back to 2017 American Transplant Congress
