Does Post-Transplant Adherence Come at a Cost?
University of Minnesota, Minneapolis, MN.
Meeting: 2016 American Transplant Congress
Abstract number: 338
Keywords: Immunosuppression, Kidney transplantation, Malignancy
Session Information
Session Name: Concurrent Session: Medication Errors, Variability and Adherence
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Room 302
Background: It is well documented that organ transplant (tx)recipients have an increased incidence of cancer including virus associated cancers like lymphoma. Our objective was to assess the correlation between immunosuppression adherence, patient's cumulative immunosuppression exposure, and incidence of cancer.
Methods: Between 1998 and 2006, 195 kidney tx recipients agreed to prospective electronic medication monitoring. Quantitative adherence to a single immunosuppressant drug (azathioprine, n=17; sirolimus, n=28; mycophenolate, n=150), averaged over 6 months was used to divide the patients into 3 equal groups (Best adherence ≥ 97.8%; Middle 91-97.7%; Worst adherence ≤ 90%). We retrospectively examined the incidence of cancer in these patients.
Results: The mean duration of follow-up (7.6 yrs) was similar in all groups. The cumulative cancer incidence was highest in the best adherent group, and lowest in the worst adherent group, p=0.029 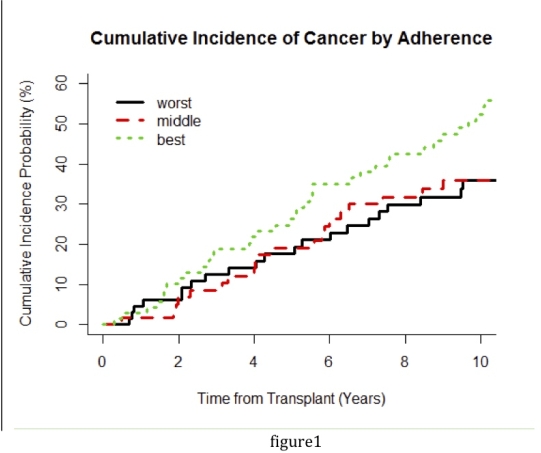 ,
,
| Cancer | Best | Midrange | Worst |
| Carcinoma | 13 | 8 | 3 |
| Hematologic (non-PTLD) | 1 | 1 | 0 |
| PTLD | 3 | 1 | 1 |
| Skin cancer | 33 | 17 | 22 |
| No cancer | 29 | 40 | 43 |
| Total patients | 69 | 61 | 65 |
. Those with the best adherence had an absolute cancer rate (per 100 pt-yrs at risk) of 6.2 cases during the first 5 yrs post-tx; , and 9.9 cases in yrs 5-10. For the least adherent group, cancer rate was 4.1 cases for the first 5 yrs; 6.0 cases in yrs 5-10. If non-melanocytic skin cancers are excluded, the cancer incidence was significantly higher in the best adherent group [p=0.011]. After adjusting for age and treating death as a competing risk, adherence grouping remained a significant factor in the incidence of cancer [p = 0.035], with the cancer hazard (vs best adherence group) 35% lower in the worst adherence group, and 49% lower in the midrange adherence group.
Conclusion:Medication adherence, although lowering AR rates and increasing long-term graft survival, is associated with increased cancer risk. Individualizing treatment to decrease the risk of either graft loss or other adverse outcomes, including malignancy, is necessary. Trials are needed to determine how to achieve this balance.
CITATION INFORMATION: Yadav K, Nevins T, Vock D, Thomas W, Robiner W, Matas A. Does Post-Transplant Adherence Come at a Cost? Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Yadav K, Nevins T, Vock D, Thomas W, Robiner W, Matas A. Does Post-Transplant Adherence Come at a Cost? [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/does-post-transplant-adherence-come-at-a-cost/. Accessed February 19, 2026.« Back to 2016 American Transplant Congress
