Discard Patterns in Donors with Non Alcoholic Fatty Liver Disease
1Surgery (Division of Surgical Transplantation), UT Southwestern Medical Center, Dallas, TX, 2Medicine (Transplant Hepatology), UT Southwestern Medical Center, Dallas, TX
Meeting: 2019 American Transplant Congress
Abstract number: 382
Keywords: Donors, marginal, Liver grafts, Liver transplantation
Session Information
Session Name: Concurrent Session: Donor Management: All Organs Excluding Kidney
Session Type: Concurrent Session
Date: Monday, June 3, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: Room 313
*Purpose: Obesity and nonalcoholic fatty liver disease (NAFLD) are major health issues affecting 20-50% of the US adult population and are increasingly prevalent in potential organ donors. We studied organ utilization in biopsy-proven NAFLD donors to understand the effect on discard and recipient outcomes.
*Methods: Scientific Registry of Transplant Recipients (SRTR) data were used to determine outcomes in adults transplanted with livers that had undergone pre-recovery donor liver biopsy between 2004 and 2018. NAFLD was defined as > 5% macrosteatosis. Co-existing donor risk factors included donor age >60 years, terminal transaminases >500 u/L, hepatitis B (HBV) core antibody positive, hepatitis C (HCV) antibody positive, donation after cardiac death (DCD), donor ICU length of stay > 7 days, and distance to transplant center >150 miles. Donor and recipient demographic data were examined, and survival and outcomes calculated. A p-value of <0.05 was considered significant.
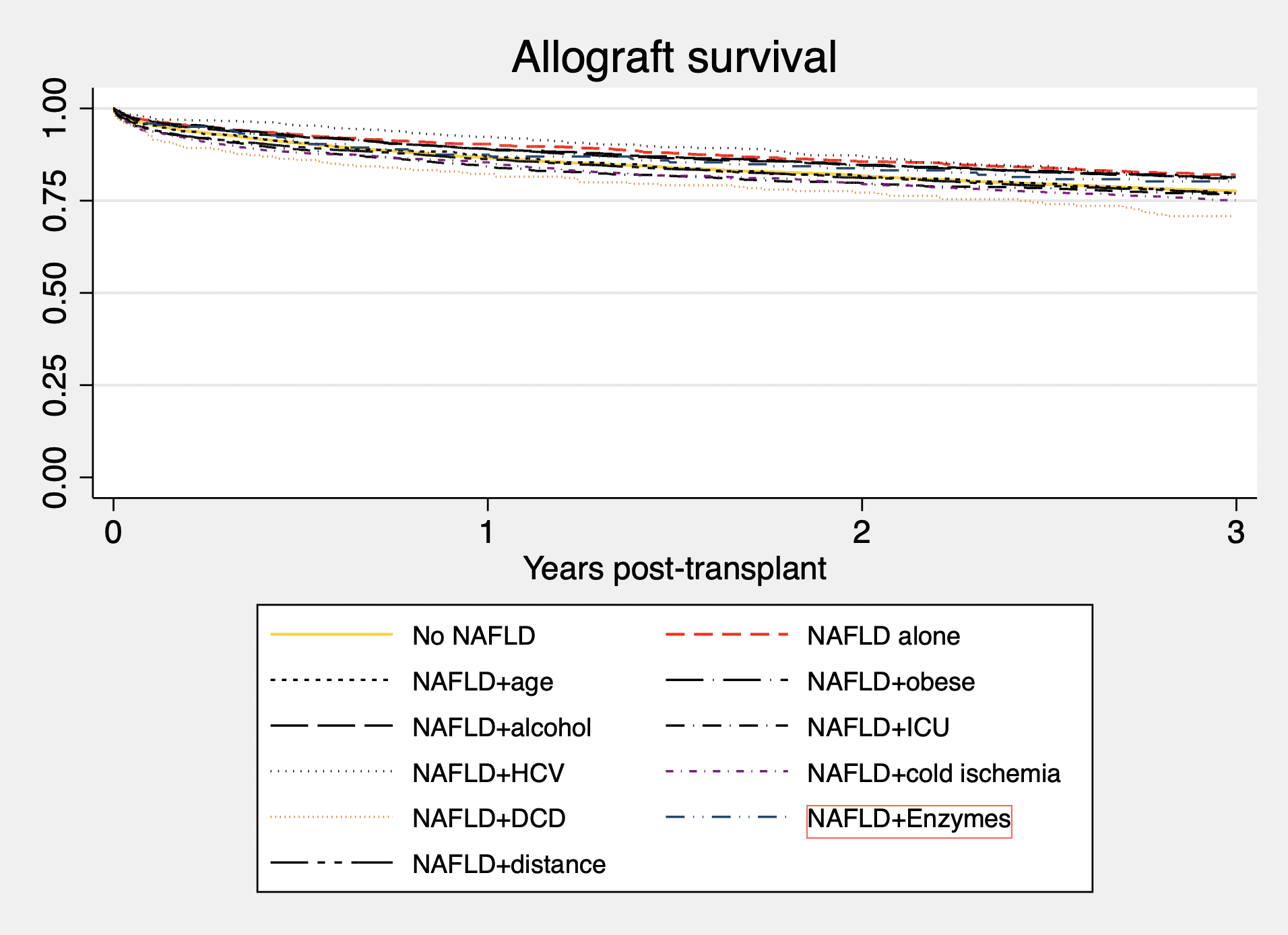
*Results: 10,275 of 38,964 (26%) of livers with a pre-recovery biopsy were not used from 2004-2017. NAFLD was noted in 6,661 (65%) of these discards, and as the primary reason for discard in 35% of donors. 21% of NAFLD donors without any additional risk were discarded. Older age (>60years), obesity (BMI >30), heavy alcohol use, prolonged donor ICU course and HCV resulted in small increases in rates of discard, however co-existing risk factors of DCD status (44.6%), elevated terminal transaminases (35.5%) and distance to transplant center (40.8%) resulted in high likelihood of discard. Allograft survival with and without NAFLD, were not significantly different. Outcomes using NAFLD livers with co-existing risk factors did not universally lead to worse outcomes, with only cold ischemia, DCD and donor ICU course combining to significantly lower long-term outcomes (Figure 1). Interestingly, there is much discordance between combinations driving discard rates and their impact on graft survival when used clinically.
*Conclusions: Biopsy findings of NAFLD, even when combined with additional co-existing donor risk factors shouldn’t trigger reflex liver discard. While there is likely selection bias underlying successful use it indicates that with appropriate recipient selection, balancing of risk can lead to good long-term outcomes.
To cite this abstract in AMA style:
MacConmara M, Mufti A, Hanish S, Vagefi P, Tujius S, Hwang C. Discard Patterns in Donors with Non Alcoholic Fatty Liver Disease [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/discard-patterns-in-donors-with-non-alcoholic-fatty-liver-disease/. Accessed March 3, 2026.« Back to 2019 American Transplant Congress