Differences in Immunosuppressive Therapy among Liver Retransplantation Recipients in a National Cohort
Hospital of the University of Pennsylvania, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: B-148
Keywords: Immunosuppression, Induction therapy, Retransplantation
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: There is no unified consensus as to the preferred immunosuppression (IS) strategy following liver retransplantation (reLT). This study explored: (i) factors associated with induction and early maintenance IS in reLT recipients, and (ii) the association of induction IS with post-reLT survival.
*Methods: This was a retrospective cohort study using the United Network for Organ Sharing database. Descriptive statistics were used to assess recipient and center factors associated with early IS strategies. Multivariable Cox proportional hazards analysis evaluated induction receipt as a predictor of post-reLT survival.
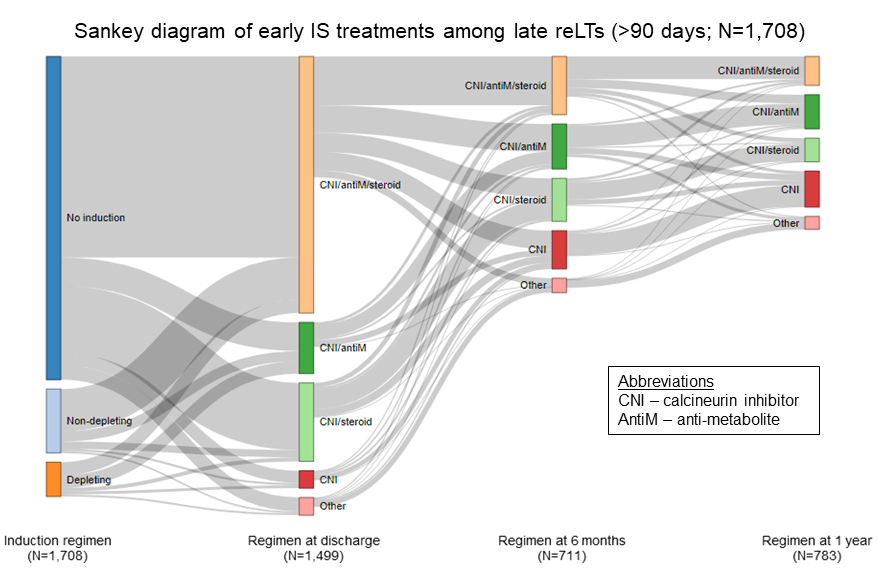
*Results: There were 3,483 adult reLT recipients from 2002-2018 at 116 centers with 95.6% being performed at the same center as the initial LT. Depleting induction was more frequently used in reLTs with prior autoimmune liver disease (27% vs 18.4% no induction; p=0.004) and reLTs >90 days from initial LT (57% vs 47.4% no induction; p<0.001). While statistically significant, differences in recipient factors between reLTs using non-depleting induction versus no induction were less pronounced. Heterogeneity in early IS practices were observed in both reLTs ≤90 versus >90 days, with the latter being shown in the Figure. Center reLT experience was associated with early IS practices. Only 11% of patients not receiving induction at initial LT were given induction at reLT. Low reLT volume centers used induction more frequently than high volume centers (28.6% vs 18.1%; p<0.001), and were also more likely to use steroid-containing regimens at 1-year (56.9% vs 37.5% high volume; p=0.005). Accounting for recipient factors and reLT center, depleting induction was an independent predictor of improved post-reLT survival: adjusted hazard ratio 0.76 (95% confidence interval 0.60-0.96 vs no induction as reference; p=0.03).
*Conclusions: While several recipient attributes inform early IS decision-making, this does not occur in a uniform manner and center factors also play a role. Further studies are needed to evaluate the impact of early IS regimens on outcomes after reLT.
To cite this abstract in AMA style:
Mezochow AK, Abt PL, Bittermann T. Differences in Immunosuppressive Therapy among Liver Retransplantation Recipients in a National Cohort [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/differences-in-immunosuppressive-therapy-among-liver-retransplantation-recipients-in-a-national-cohort/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress