Diabetes is a Significant and Independent Predictor for Tacrolimus Immediate Release (IR) and LCP-Tacrolimus (LCP) Conversion Ratios
K. S. Coffman, N. Patel, F. Bartlett, J. Newman, S. Patel, T. Sprague, N. Rao, E. Andrade, M. Casey, V. Rohan, D. DuBay, D. Taber
Medical University of South Carolina, Charleston, SC
Meeting: 2022 American Transplant Congress
Abstract number: 773
Keywords: Immunosuppression, Kidney transplantation, Metabolic disease, Post-transplant diabetes
Topic: Clinical Science » Kidney » 35 - Kidney: Cardiovascular and Metabolic Complications
Session Information
Session Name: Kidney: Cardiovascular and Metabolic Complications
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Diabetes (DM) is a common comorbidity seen in transplant patients with known effects on GI motility and absorption; however, DMs impact on the IR tacrolimus to LCP-tacrolimus (LCP) conversion ratio has not been studied.
*Methods: This was a multivariable analysis of a retrospective longitudinal cohort study including patients converted from IR to LCP between 2017 and 2019 with follow up through 2021. The primary outcome was IR to LCP conversion ratio based on presence or absence of DM (pre-existing or new onset). Other outcomes included tacrolimus variability using the coefficient of variation (CV), time in therapeutic range, adverse events, infection (BK, CMV), development of donor specific antibodies, rejection, graft loss, and death.
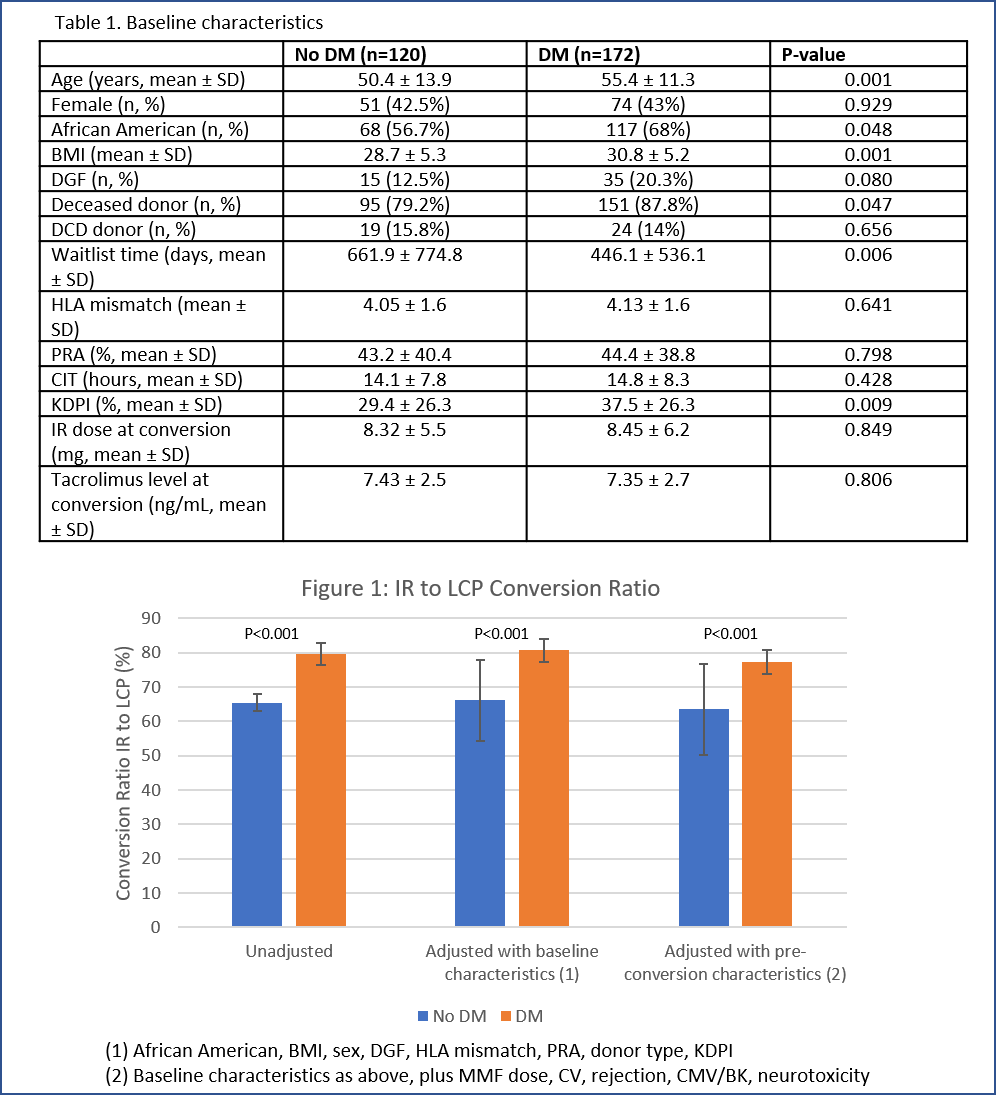
*Results: A total of 292 patients were included; 120 without DM and 172 patients with DM (either pre-existing DM or NODAT). Baseline characteristics were similar, with exceptions of African American race (56.7% vs. 68%), pancreas transplant (0 vs. 8.7%), and BMI (28.7 vs. 30.8). The IR to LCP conversion ratio was significantly higher in patients with DM (67.5% ± 21.1% vs. 79.8% ± 28.7%; P < 0.001). In multivariable modeling, DM was the only variable significantly and independently associated with IR to LCP conversion ratio. Higher conversion ratios with DM were consistent across unadjusted and fully adjusted models (see figure). No difference was seen in rejection rates based on DM status. Graft survival was lower in the DM patients (97.5% vs. 92.4%; P=0.062), as was patient survival (100% vs. 94.8%; P=0.011).
*Conclusions: The presence of DM significantly increased the IR to LCP conversion ratio by 13 to 14%, as compared to patients without DM. On multivariable analysis, DM was the only significant predictor of conversion ratios, potentially related to GI motility or absorption differences. Future studies are warranted to assess the mechanism of conversion ratio differences by DM status, while assessing clinical implications of this as well.
To cite this abstract in AMA style:
Coffman KS, Patel N, Bartlett F, Newman J, Patel S, Sprague T, Rao N, Andrade E, Casey M, Rohan V, DuBay D, Taber D. Diabetes is a Significant and Independent Predictor for Tacrolimus Immediate Release (IR) and LCP-Tacrolimus (LCP) Conversion Ratios [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/diabetes-is-a-significant-and-independent-predictor-for-tacrolimus-immediate-release-ir-and-lcp-tacrolimus-lcp-conversion-ratios/. Accessed February 22, 2026.« Back to 2022 American Transplant Congress