Determinants and Sequelae of Hepatic Artery Thrombosis After Liver Transplantation: A Registry Study of Recipient Diagnosis and Coagulopathy
1Washington University, Barnes Jewish Hospital, Saint Louis, MO
2Johns Hopkins University, Johns Hopkins Hospital, Baltimore, MD.
Meeting: 2015 American Transplant Congress
Abstract number: 106
Keywords: Hepatic artery, Liver transplantation, Outcome, Risk factors
Session Information
Session Name: Concurrent Session: Liver Retransplantation and Other Complications
Session Type: Concurrent Session
Date: Sunday, May 3, 2015
Session Time: 4:00pm-5:30pm
 Presentation Time: 4:24pm-4:36pm
Presentation Time: 4:24pm-4:36pm
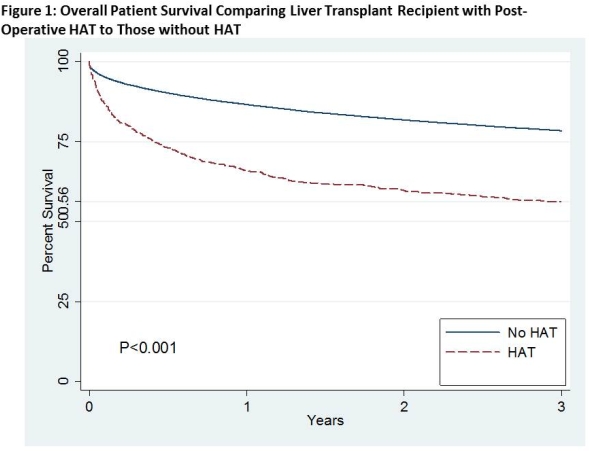
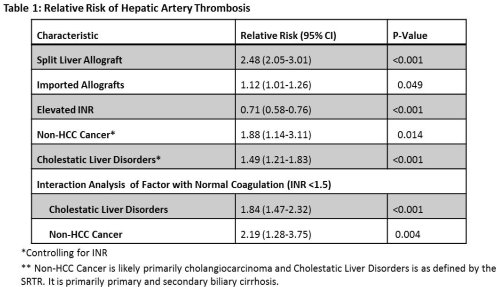
Location: Room 115-AB
Hepatic artery thrombosis (HAT) is a dreaded complication following liver transplantation. Despite improvements in technique and procurement, HAT still occurs in approximately 2-5% of recipients. We explored registry data to identify risk factors associated with HAT. We used United Network for Organ Sharing (UNOS) data from 2000-2010 to study adult liver transplant recipients. Kaplan-Meier methodology and Cox proportional hazards models were used to calculate the association between HAT and patient survival. Interaction term analysis was used to evaluate the role of both coagulopathy and cause of liver disease on HAT. Among 50,723 adult liver transplant recipients, 814 patients developed HAT. HAT was associated with a 2.24-fold increased risk of death [Figure 1]. Coagulopathy was protective for HAT (RR 0.71, 95% CI 0.58-0.76, p <0.001). On average, split liver allograft (RR 2.48, 95% CI 2.05-3.01, p <0.001), non-HCC associated liver cancer (RR 1.88, 95% CI 1.14-3.11, p =0.014), and cholestatic liver disorders (RR 1.49, 95% CI 1.21-1.93, p <0.001) were associated with HAT. However, the effect of these risk factors was more pronounced in those with normal coagulation: the risk of HAT associated with cholestatic liver disease was 1.84 times higher in patients with normal coagulation compared to those with coagulopathy, and the risk associated with non-HCC associated liver cancer was 2.19 times higher in those with normal coagulation compared to those with coagulopathy [Table 1]. These findings may warrant consideration of anticoagulation measures in carefully selected high risk patients.
To cite this abstract in AMA style:
Wang JGaronzik, Doyle M, Collins K, Lowell J, Lin Y, Shenoy S, Wellen J, Chapman W, Segev D. Determinants and Sequelae of Hepatic Artery Thrombosis After Liver Transplantation: A Registry Study of Recipient Diagnosis and Coagulopathy [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/determinants-and-sequelae-of-hepatic-artery-thrombosis-after-liver-transplantation-a-registry-study-of-recipient-diagnosis-and-coagulopathy/. Accessed February 17, 2026.« Back to 2015 American Transplant Congress
