Decoding the Troubled Allograft: Proteinuria within the 1st Post-Transplant Year Associates with and Risk Stratifies Inflamed Renal Transplants
Starzl Transplantation Institute, UPMC, Pittsburgh, PA
Meeting: 2020 American Transplant Congress
Abstract number: 455
Keywords: Graft failure, Proteinuria, Rejection
Session Information
Session Name: Kidney Complications: Immune Mediated Late Graft Failure
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:27pm-4:39pm
Presentation Time: 4:27pm-4:39pm
Location: Virtual
*Purpose: The relationship between progression of proteinuria and allograft histology through the 1st year with clinical outcomes is unclear.
*Methods: Here, we systematically studied proteinuria {early (<4mo) or late (at 1yr) using uPCR} and allograft histology in 1000 patients transplanted between 2013-17. Patients were divided into 4 groups based on proteinuria evolution (Gp-I: <0.5g thru 1yr; Gp-II: >0.5g early &<0.5g by 1yr; Gp-III: <0.5g early & >0.5g by 1yr; Gp-IV: proteinuria>0.5g thru 1yr). IS utilized Thymo followed by Tac+MMF. Patients underwent 2 protocol biopsies (Bx) at 3mos & 1yr and any for-cause Bx. Importantly uPCR was assessed at each Bx. Patients with de novo or recurrent GN were excluded
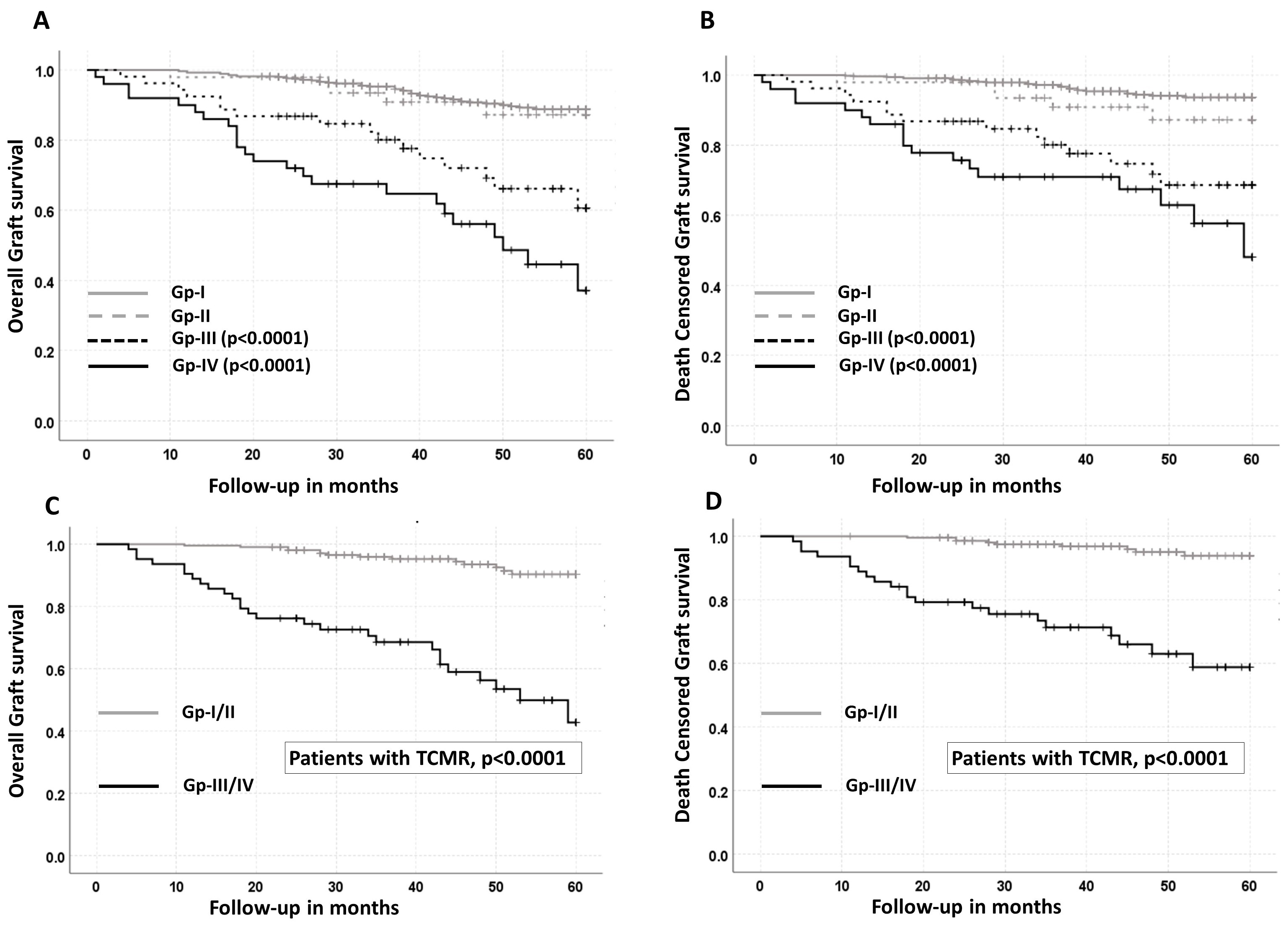
*Results: Proteinuria: Of the 800 patients with 1287 matched Bx to proteinuria, 78% were in Gp-I, while 7% were in Gp-II and 7.5% each in Gp-III & IV. Thus 15% of the patients had either evolving or persistent proteinuria. Gp III & IV was associated with worse graft loss at 5yrs compared to Gp I & II independent of sCr at 1yr (HR, 3.8, 95% CI 2.4-6.1, p<0.0001), thus representing a high-risk category (Fig1A/B). Proteinuria and Histology: Gp III/IV was associated with significantly worse t, i, g & ptc Banff scores both early and late when compared to Gp I/II. This translated not only to 2 X increased TCMR in Gp III/IV at both time points compared to Gp-I/II (Early: 45% vs. 23%, p<0.0001; Late: 58% vs. 27%, p<0.0001) but also greater severity. Further, Gp-III/IV was associated with a 3.9 X increased odds of recurrent/recalcitrant TCMR compared to Gp-I/II (95% CI 1.7-9.1, p=0.0006) despite therapy. Next, Gp-III/IV was associated with worse IFTA compared to Gp-I/II (IFTA score: 1.8 vs. 2.72, p<0.0001; IFTA≥3, Gp I/II 15% vs. Gp III/IV 29%, p<0.0001). Thus persistent/evolving proteinuria associates with worse allograft inflammation through the 1st year and increased scarring at 1yr. Histology, proteinuria and outcomes: Allograft inflammation (TCMR), in combination with Gp III/IV proteinuria was associated with markedly worse outcomes independent of potential confounders including serum sCr at 1yr (overall graft survival, HR, 6.5, 95% CI 3.2-13.2, p<0.0001; death censored graft survival, HR 6.8, 95% CI 2.8-16.1, p<0.0001) (Fig 1C/D).
*Conclusions: Early proteinuria >0.5g associates with worse allograft inflammation and in combination identifies a sub-group of patients at risk for poor graft outcomes. Such patients could represent a target population for future clinical trials with novel agents aimed at improving outcomes.
To cite this abstract in AMA style:
Cherukuri A, Mehta R, Tevar A, Munjal R, Kalra K, Puttarajappa C, Sood P, Wu C, Hariharan S. Decoding the Troubled Allograft: Proteinuria within the 1st Post-Transplant Year Associates with and Risk Stratifies Inflamed Renal Transplants [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/decoding-the-troubled-allograft-proteinuria-within-the-1st-post-transplant-year-associates-with-and-risk-stratifies-inflamed-renal-transplants/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress