Declining Inpatient Mortality for Patients with Human Immunodeficiency Virus (HIV) and Cirrhosis: A Temporal Analysis of the Nationwide Inpatient Sample
Weill Cornell Medicine, New York, NY
Meeting: 2020 American Transplant Congress
Abstract number: A-115
Keywords: HIV virus, Liver, Liver cirrhosis
Session Information
Session Name: Poster Session A: Liver: Portal Hypertension and Other Complications of Cirrhosis
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Despite the advent of highly effective anti-retroviral therapy, HIV remains a major health burden. Though life expectancy has improved, patients are now dying from non-HIV comorbidities such as cirrhosis. This study examined mortality trends of patients hospitalized with cirrhosis and HIV over time using a nationally representative hospital database.
*Methods: Hospitalized adults with cirrhosis, identified by a validated algorithm, were included using the Nationwide Inpatient Sample from 2000-2014. Discharges were weighted to give nationally-representative estimates. The primary outcome was inpatient mortality over time among patients with HIV and cirrhosis compared to patients with cirrhosis alone. Secondary outcomes included admissions for decompensating liver-related events and infection. Predictors for mortality, including infection-related mortality, were also determined by multivariable logistic regression controlling for covariates selected a priori.
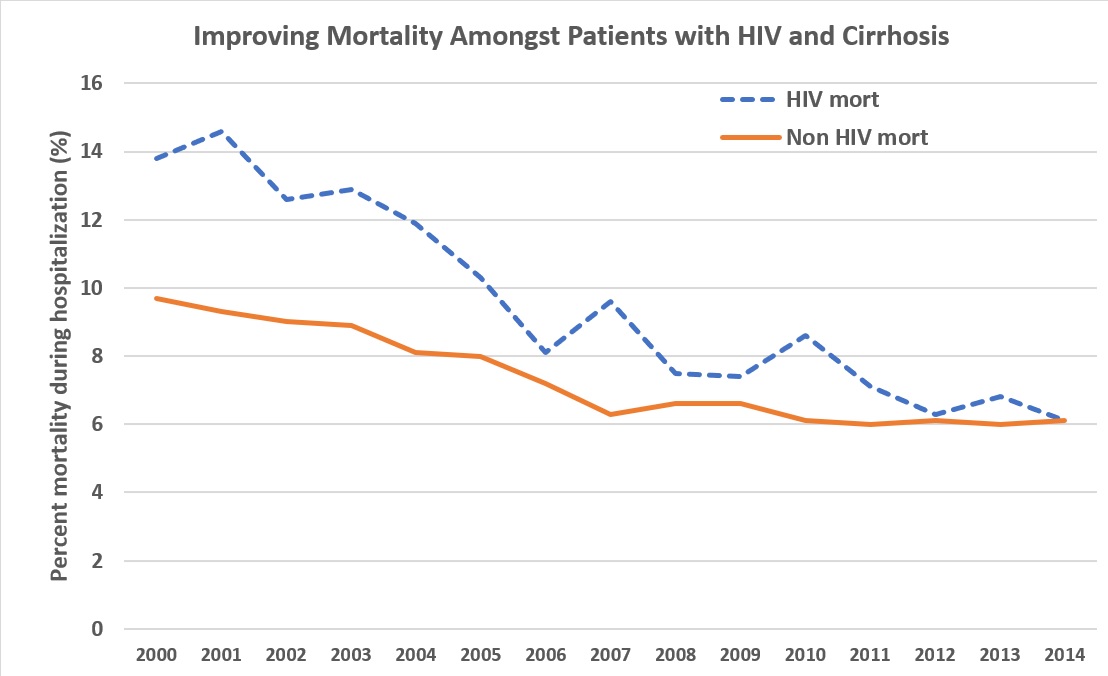
*Results: Of the 6,142,750 weighted discharges included, 119,161 (1.9%) patients had cirrhosis and HIV. Inpatient mortality for those with HIV and cirrhosis decreased from 13.8% in 2000 to 6.1% in 2014 and is now equivalent to non-HIV.
Compared to those without HIV, patients with HIV and cirrhosis had fewer decompensating events including ascites, encephalopathy, and gastrointestinal bleeding (37% vs. 44%), but higher rates of infection (27% vs. 25%), both p<0.001. In multivariable analysis, HIV was an independent predictor of overall mortality (OR 1.66, 95% CI 1.58-1.73, p<0.001) and infection-related mortality (OR 1.55, 95% CI 1.45-1.65).
| Variable | Overall mortality | Infection-related mortality | ||
| Adjusted OR | P-value | Adjusted OR | P-value | |
| HIV | 1.66 (1.58-1.73) | <0.001 | 1.55 (1.45-1.65) | <0.001 |
| Ascites | 1.53 (1.51-1.56) | <0.001 | 1.33 (1.30-1.36) | <0.001 |
| Hepatic encephalopathy | 2.63 (2.59-2.68) | <0.001 | 2.01 (1.96-2.06) | <0.001 |
| Gastrointestinal bleeding | 1.91 (1.88-1.94) | <0.001 | 1.92 (1.87-1.96) | <0.001 |
*Conclusions: Inpatient mortality in patients with cirrhosis and HIV has dramatically decreased and now equals that of non-HIV patients. However, HIV still remains an independent predictor of mortality and infection-related mortality, and points to a need for early identification and effective treatment of infections within this high risk hospitalized population.
To cite this abstract in AMA style:
Kaplan A, Lucero C, Fortune B, Jesudian A, Jr RSBrown, Rosenblatt R. Declining Inpatient Mortality for Patients with Human Immunodeficiency Virus (HIV) and Cirrhosis: A Temporal Analysis of the Nationwide Inpatient Sample [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/declining-inpatient-mortality-for-patients-with-human-immunodeficiency-virus-hiv-and-cirrhosis-a-temporal-analysis-of-the-nationwide-inpatient-sample/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress