De Novo Atypical Hemolytic Uremic Syndrome (aHUS) in Kidney Transplant Recipients from the Same Donor: Possible Role of Two Genetic Hits
1University of California at San Diego, San Diego, CA, 2University of Utah School of Medicine, Salt Lake City, UT, 3Nephrology Associates of Utah, Salt Lake City, UT
Meeting: 2021 American Transplant Congress
Abstract number: 1051
Keywords: Graft function, Kidney
Topic: Clinical Science » Kidney » Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Thrombotic microangiopathy (TMA) is an uncommon and potentially serious complication of kidney transplantation. Atypical hemolytic uremic syndrome (aHUS) is a type of TMA most often occurring as a result of dysregulation in the alternative complement pathway. While aHUS can manifest as recurrent disease following a kidney transplant, de novo post-transplant aHUS is uncommon and poorly understood.
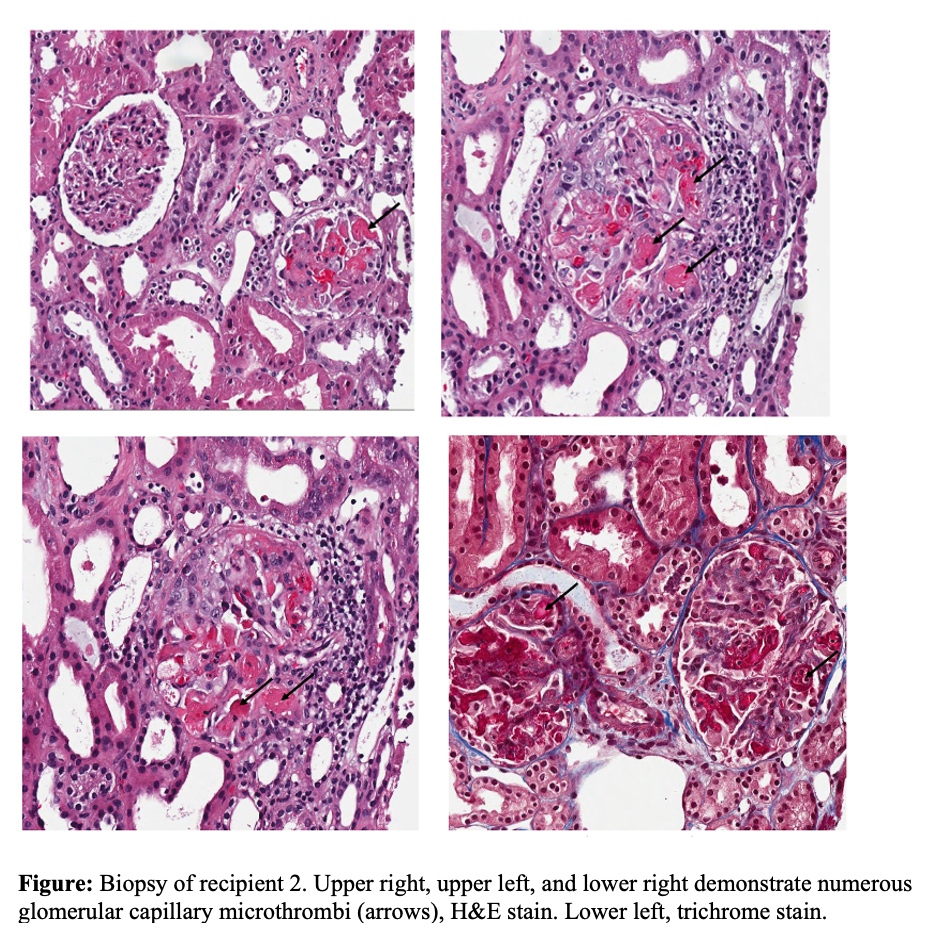
*Methods: We describe two cases of de novo aHUS occurring in both kidney transplant recipients from the same deceased donor. Recipient 1 was a 3-year-old male with ESRD due to bilateral dysplastic kidneys. Immediately following transplant, he had slow graft function complicated by severe TMA that resolved following administration of eculizumab. Genetic testing later revealed a variant in membrane-cofactor protein (MCP) thought to have a low likelihood of being related to the development of aHUS. Recipient 2 was a 33-year-old female with a history of ESRD of unknown etiology who also developed TMA in the immediate post-transplant period. A kidney biopsy was consistent with TMA and her condition resolved following administration of eculizumab (figure). A genetic panel for aHUS later revealed a homozygous deletion for complement factor H related proteins, associated with Factor H antibodies and aHUS. However, Factor H antibodies were not detected in the patient. Genetic testing was later obtained from donor tissue, revealing a variant in C3 of debatable significance.
*Results: Neither donor nor receipts had evidence of TMA prior to transplantation. The possible explanation and trigger lies in the donor C3 mutation. We conjecture the donor variant C3 is a gain of function mutation which led to pre-donation setup of complement activation in the deceased donor with ischemia. Additionally, complement activation with surgery as a trigger in the immediate post-transplant period resulted in further allograft C3 expression with increased resistance to Factor H and MCP (due to recipients mutations). The overactive and uninhibited C3 resulted in downstream inflammation and endothelial damage leading to the aHUS phenotype in both recipients. We report for the first time, a two genetic hit scenario leading to de novo aHUS in two separate kidney transplant recipients from same deceased donor.
*Conclusions: The case highlights the importance of obtaining genetic tests from deceased donor tissue to evaluate possible mechanisms in cases of de novo genetically mediated disease.
To cite this abstract in AMA style:
Crane C, Sherbotie J, Anand S. De Novo Atypical Hemolytic Uremic Syndrome (aHUS) in Kidney Transplant Recipients from the Same Donor: Possible Role of Two Genetic Hits [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/de-novo-atypical-hemolytic-uremic-syndrome-ahus-in-kidney-transplant-recipients-from-the-same-donor-possible-role-of-two-genetic-hits/. Accessed February 22, 2026.« Back to 2021 American Transplant Congress