Covid-19 Caseload and Management Practices Vary by Program-Level Factors: A Multinational Survey Study
S. Sandal1, B. Boyarsky2, P. Chiang2, A. Massie2, D. Segev2, M. Cantarovich1
1McGill University, Montreal, QC, Canada, 2Johns Hopkins University, Baltimore, MD
Meeting: 2021 American Transplant Congress
Abstract number: 764
Keywords: Infection, Multicenter studies, N/A
Topic: Clinical Science » Infectious Disease » All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: All Infections (Excluding Kidney & Viral Hepatitis)
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: During the pandemic, the COVID-19 patient caseload (CPC) is thought to be highly variable and likely dependant on the cumulative COVID-19 incidence (CCI) of the region. We aimed to capture this variability and COVID-19 treatment practices during the early months of the pandemic.
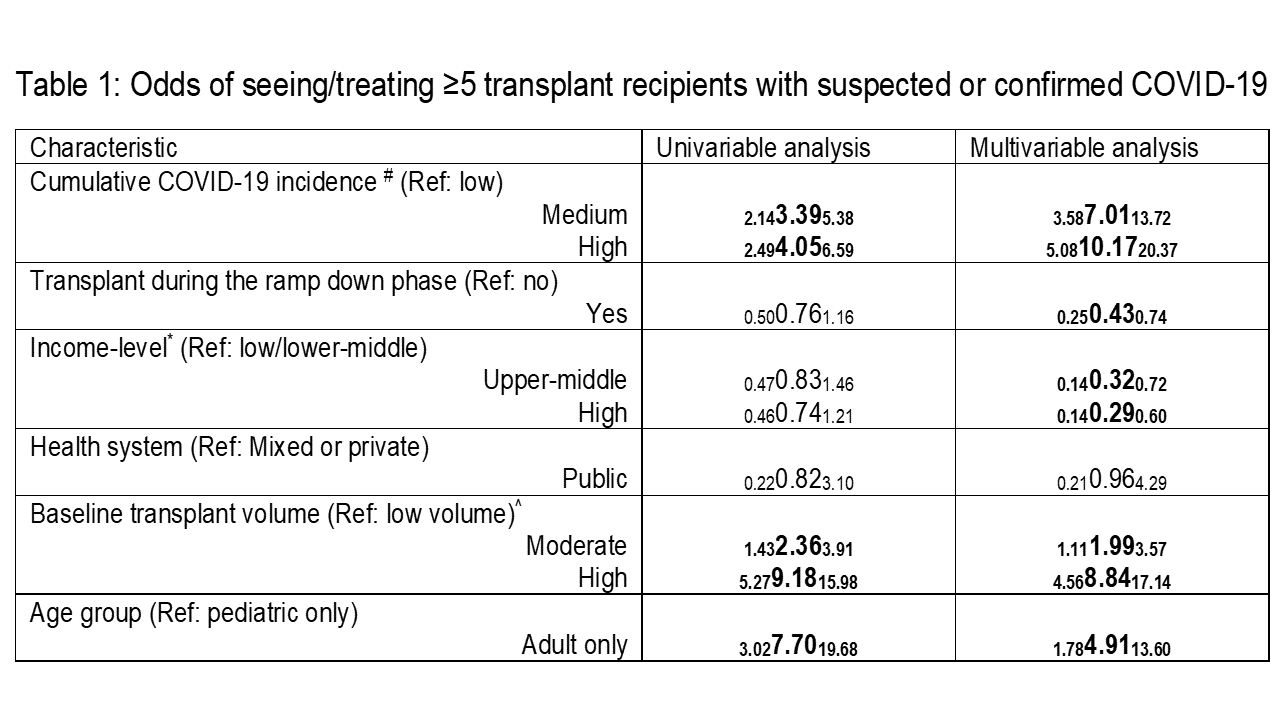
*Methods: From June-September 2020, we conducted a multinational survey of transplant physicians. Of 1,267 physicians contacted, 40.5% from 71 countries participated. CCI was calculated in person per million population (ppm) from March-July and divide into tertiles for the entire cohort (low: <2031ppm, medium: 2032-5400ppm, high: >5400ppm). The primary outcome of interest was a CPC of ≥5 transplant recipients. Logistic regression was used to conduct a comparative analysis. We also asked centers to report their treatment practices by patient symptoms, and rate the likelihood of recommending these treatments on a scale of 1-5 (1 being very unlikely and 5 being very likely).
*Results: 70.6% of programs reported seeing recipients with COVID-19 (31.0% <5, 16.2% 5-10, 13.5% 11-20, 6.4% 21-50, and 3.5% >50 cases). When compared with transplant programs from areas with low CCI, those from medium and high CCI areas had 7- and 10-times higher odds of ≥5 CPC, respectively. When compared with low/lower-middle-income countries, upper-middle-income countries and high-income countries had 68% and 71% lower odds for this outcome. More importantly, performing a transplant during this time was associated with 54% lower odds of a higher COVID-19 caseload. In terms of treatments, while reducing immunosuppression was the mainstay, in patients with mild and moderate symptoms, supportive care only (59.3% vs. 23.2%), azithromycin (14.8% vs. 22.8%), and hydroxychloroquine/chloroquine (11.3% vs.17.2%) were the top three choices. In patients with severe symptoms, a wide range of treatments was reported. Supportive care only (4.13±1.22) and Remdesivir (4.13±0.94) were strongly recommended by those that used them.
*Conclusions: The CPC is strongly associated with the CCI and income level of a region. But performing a transplant during the early days of the pandemic was not associated with seeing more patients with COVID-19. In transplant recipients with COVID-19, supportive care only and decreasing maintenance immunosuppression are the mainstays of therapy. Should there be a second wave of the pandemic, our findings may help guide clinical practice.
To cite this abstract in AMA style:
Sandal S, Boyarsky B, Chiang P, Massie A, Segev D, Cantarovich M. Covid-19 Caseload and Management Practices Vary by Program-Level Factors: A Multinational Survey Study [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/covid-19-caseload-and-management-practices-vary-by-program-level-factors-a-multinational-survey-study/. Accessed February 27, 2026.« Back to 2021 American Transplant Congress