Combined Heart-Liver Transplantation for Failing Fontan Physiology: A Large Single Center Comparative Analysis
1Liver and Pancreas Transplant Center, UCLA, Los Angeles, CA, 2Ahmanson/UCLA Adult Congenital Heart Disease Center, UCLA, Los Angeles, CA, 3Cardiac Surgery, UCLA, Los Angeles, CA, 4Cardiology, UCLA, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 147
Keywords: Heart failure, Heart transplant patients, Liver transplantation, Surgery
Topic: Clinical Science » Heart » 63 - Heart and VADs: All Topics
Session Information
Session Name: Heart and VADs: All Topics I
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:40pm-6:50pm
Presentation Time: 6:40pm-6:50pm
Location: Hynes Room 210
*Purpose: The rate of combined heart-liver transplantation (HLT) has tripled in the last decade, and continues to rise along with the number of patients with a failing Fontan palliation. Cardiac failure with congestive liver disease is fueling demand for HLT in this complex patient population. We examined post-Fontan HLT (FHLT) patients compared to patients without congenital heart defects receiving HLT, or post-Fontan patients receiving heart transplant (FHT) alone.
*Methods: HLT, FHLT and FHT recipients were compared [35 patients, retrospective, single center; 2004-2020]. Analysis was done using SPSS Statistics 27. Pre, intra and post-operative variables were examined.
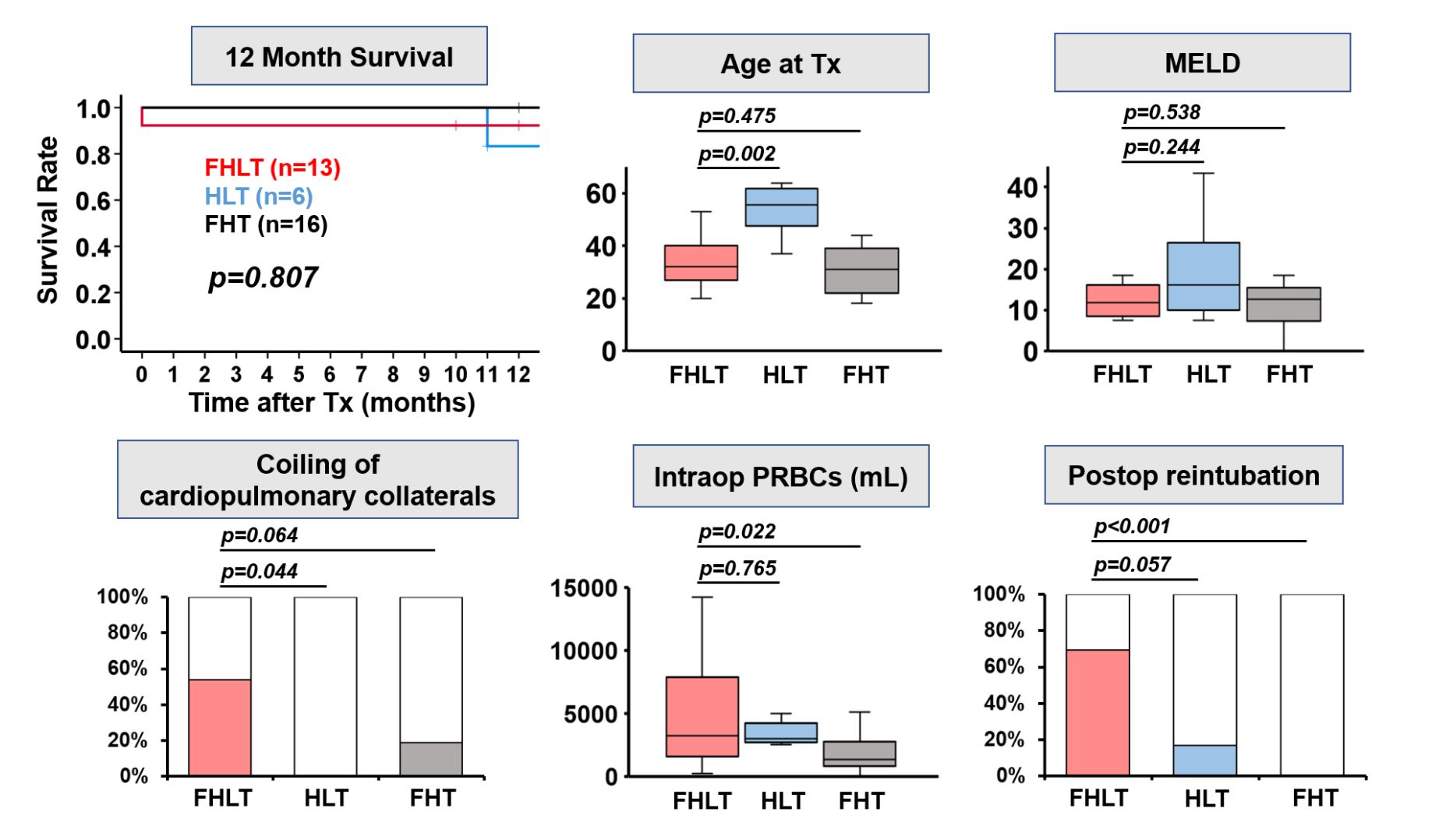
*Results: Within post-Fontan patients, there were 13 FHLT and 16 FHT. 6 patients received HLT. Compared to HLT patients, FHLT patients were significantly younger (median age: 32.5 vs. 55.5, p=0.002) and had more prior sternotomies (median 3 vs. 0, p<0.001). Relative to FHT patients, FHLT patients had longer preoperative hospital stay (median days: 50 vs. 12.5, p=0.001), higher incidence of bridging fibrosis on preoperative biopsy (69.2% vs. 18.8%, p=0.006), and greater intraoperative transfusion requirements (median mL PRBC: 3250 vs. 1350, p=0.022). Compared to either group, FHLT patients had more prior coiling procedures (53.8% vs. 0% HLT, p=0.044, 53.8% vs. 18.8% FHT, p=0.064), a greater proportion of NYHA class IV patients (100% vs. 33% HLT, p=0.087, 100% vs. 43.8% FHT, p=0.062), and more frequent postoperative reintubation (69.2% vs. 16.7% HLT, p=0.057, 69.2% vs. 0% FHT, p<0.001). Two FHLT patients had hepatocellular carcinoma, compared to none in the other groups. All groups had similar MELD scores, postoperative hospital stays, and one-year survival (FHLT 83.3%, HLT 92.3%, FHT 100%, p=0.807).
*Conclusions: This represents one of the largest single center studies in patients with a failing Fontan receiving HLT. These patients are more challenging to manage compared to non-congenital HLT and post-Fontan HT patients. Although post-Fontan HLT patients have greater perioperative care needs, their outcomes are comparable to these other patient groups. Rising utilization of HLT as a life-saving operation in patients with a failing Fontan requires continued attention to further optimize outcomes in these complex patients.
To cite this abstract in AMA style:
Rosenthal CJ, Noguchi D, Aboulhosn JA, Arsdell GSVan, Nsair A, Ha M, Reardon L, Lluri G, Lin JP, Saab S, Baird A, Venick RS, Farmer DG, Kaldas FM. Combined Heart-Liver Transplantation for Failing Fontan Physiology: A Large Single Center Comparative Analysis [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/combined-heart-liver-transplantation-for-failing-fontan-physiology-a-large-single-center-comparative-analysis/. Accessed February 23, 2026.« Back to 2022 American Transplant Congress