CMV Risk Status Remains a Relevant Risk Factor for Long-Term Outcomes
Emory University, Atlanta, GA
Meeting: 2019 American Transplant Congress
Abstract number: 10
Keywords: Cytomeglovirus, Kidney transplantation, Risk factors, Survival
Session Information
Session Name: Concurrent Session: Kidney Complications: Late Graft Failure I
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Veterans Auditorium
*Purpose: Intensification of immunosuppression using T cell depleting induction has reduced rates of acute cellular rejection after kidney transplantation. Belatacept, a first in class T cell costimulation blocker avoids CNI nephrotoxicity, inhibits donor specific antibody formation and improves survival after kidney transplant. While offering advantages in controlling alloimmunity these approaches perturb protective immunity. Despite the use of antiviral agents CMV remains a source of morbidity. We sought to understand the impact of cmv risk status on survival outcomes using current immunosuppressive regimens.
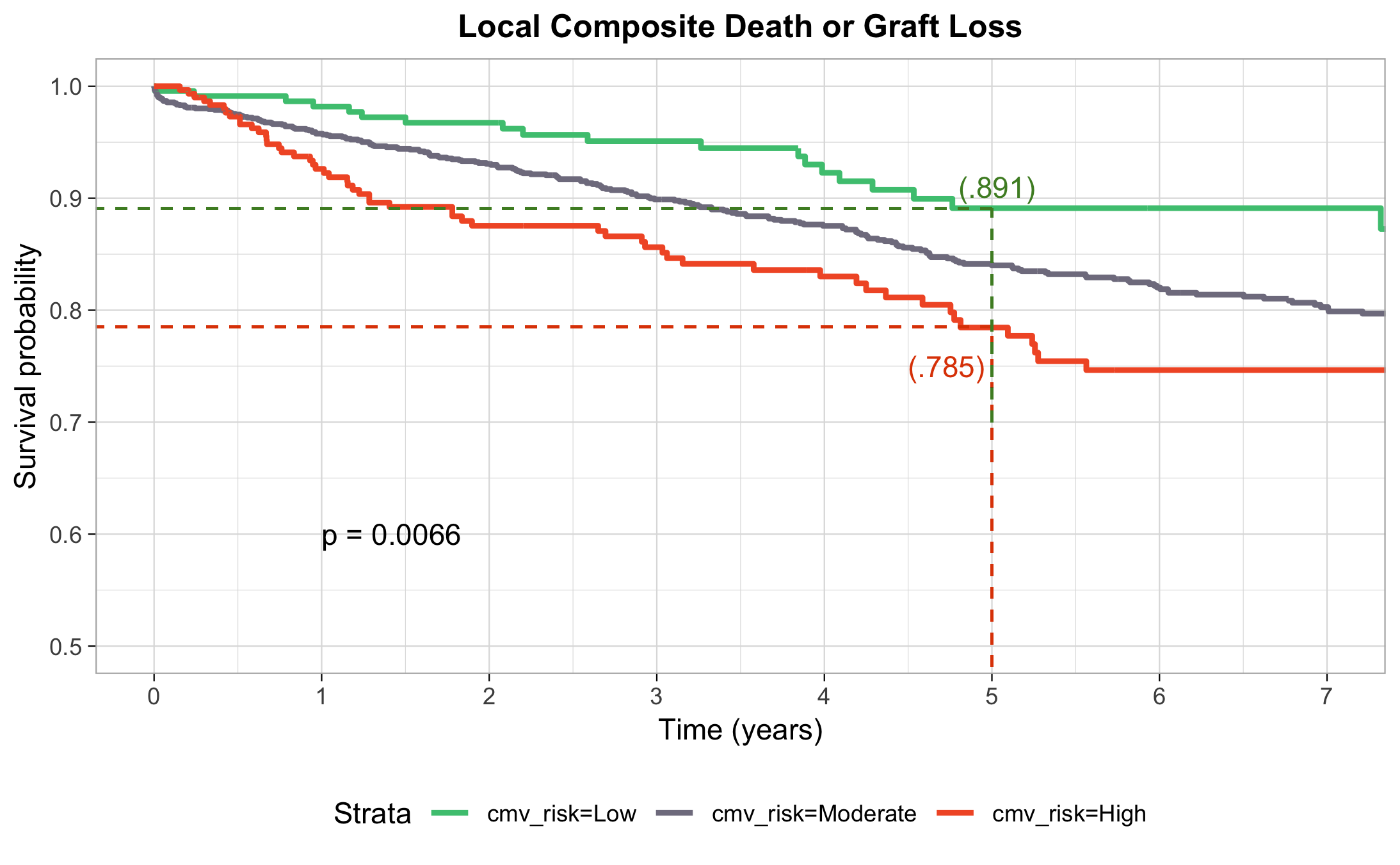
*Methods: To determine impact of cmv risk status on kidney transplant survival outcomes (death, death censored graft loss or a composite of the two) in the US we analyzed primary kidney transplants performed between 2006-2017 using data from SRTR and our local program data. Descriptive statistics, Kaplan-Meier (KM) and Cox model analyses were performed with R (survival and survminer).
*Results: The SRTR cohort consisted of 99,312 recipients of deceased (dd) and 52,643 living donor (ld) kidneys. Distribution by CMV risk status was low 17%, moderate 65% and high 18%. Our local cohort contained 2124 dd and 762 ld recipients with similar CMV risk. KM analysis (Fig 1 and 2) showed a significant difference by CMV risk status for each data set (p< 0.01). In SRTR data CMV high risk was status was a significant predictor of each of the survival outcomes in Cox proportional hazard and adjusted survival while including donor type, race, induction type and recipient age in the model (HR 1.19, p < 0.007). Donor type, race but not induction were also significant in the model. In our local data CMV high risk was also an independent predictor of survival (HR 2.07, p 0.024) as was donor type, but not race or use of belatacept vs. tacrolimus.
*Conclusions: CMV high risk status remains an important predictor of morbidity and mortality in the current era irrespective of induction or primary maintenance therapy. Further study of the duration, magnitude, and recurrence of viremia by induction and maintenance should be undertaken. Directing organs from CMV negative deceased and or living donors to CMV negative recipients could improve survival. Studies to model to impact on survival, cost and waiting time should be considered.
To cite this abstract in AMA style:
Karadkhele G, Zhang W, Larsen CP. CMV Risk Status Remains a Relevant Risk Factor for Long-Term Outcomes [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/cmv-risk-status-remains-a-relevant-risk-factor-for-long-term-outcomes/. Accessed February 19, 2026.« Back to 2019 American Transplant Congress