Clinically Adjudicated Deceased Donor AKI and Graft Outcomes
1Yale, New Haven, CT, 2Utah Univ, Salt Lake City, UT, 3UPenn, Philadelphia, PA, 4Columbia, New York, NY, 5Univ of Michigan, Ann Arbor, MI, 6Drexel, Philadelphia, PA, 7Univ of Maryland, College Park, MD, 8Cornell, NY, NY, 9Thomas Jefferson, Philadelphia, PA, 10Johns Hopkins, Baltimore, MD, 11Montefiore, Bronx, NY, 12St Barnabas, Livingston, NJ, 13Univ Hosp, Ulm, Germany
Meeting: 2020 American Transplant Congress
Abstract number: 12
Keywords: Graft function, Kidney transplantation
Session Information
Session Name: Kidney Deceased Donor Allocation I
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: We previously reported that AKI in deceased donors isn’t associated with graft failure. As deceased donors undergo significant hemodynamic changes, we hypothesized that reversible hemodynamic abnormalities lead to most cases of deceased-donor AKI and may explain lack of association with graft failure.
*Methods: In this ancillary study of the Deceased Donor Study, a random sample of 428 donors with available charts was selected to identify donors with and without AKI defined as 0.3 mg/dL increase in creatinine at any time during hospitalization from the lowest value. Three nephrologists, blinded to outcomes, reviewed AKI donor charts to classify as hemodynamic (hAKI), intrinsic (iAKI), or mixed (mAKI). Majority adjudication determined final diagnosis. If all disagreed AKI was adjudicated as mAKI. We evaluated the associations between AKI phenotypes happening at any time during hospitalization with the outcomes of delayed graft failure (DGF) and 1-year eGFR. In secondary analysis, we evaluated these associations in a subset of donors with ongoing AKI at time of procurement, as current allocation decisions focus on terminal serum creatinine.
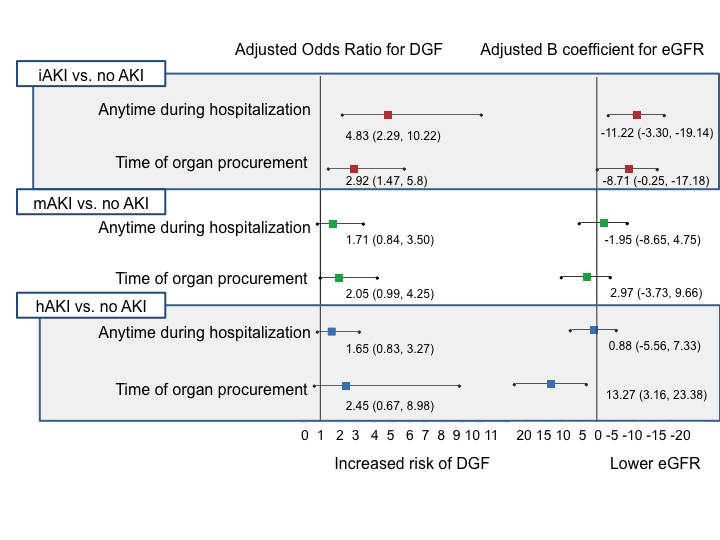
*Results: Nephrologists adjudicated 106 (36%) donors as having hAKI, 84 (29%) as iAKI and 101 (35%) as mAKI. 137 didn’t meet clinical definition of AKI. A total of 669 kidneys were transplanted with 32% having DGF and a median 1-year eGFR of 53 (IQR: 41-70). Donors with iAKI at any time during hospitalization had higher DGF and lower 1-year eGFR as compared to non AKI (figure). In a subset of 124 donors, AKI was ongoing at the time of procurement and included 13% hAKI, 36% mAKI and 51% iAKI. Donors with iAKI had higher DGF and lower 1-year eGFR compared to non AKI. In contrast donors with hAKI had higher 1-year eGFR at time of procurement.
*Conclusions: Intrinsic AKI, occurring earlier during donor hospitalization or ongoing at time of organ procurement is associated with higher DGF and lower 1-year eGFR. Higher 1-year eGFR was noted for kidneys with hAKI at time of organ procurement. Clinically phenotyped deceased donor AKI may help inform deceased donor organ allocation.
To cite this abstract in AMA style:
Mansour SG, Khoury N, Vermani S, Koladi R, Hall I, Reese P, Mohan S, Doshi M, Harhay M, Bromberg J, Thangamani M, Singh P, Jia Y, Thiessen-Philbrook H, Akalin E, Weng F, Schroeppel B, Greenberg J, Moledina D, Wilson FP, Parikh C. Clinically Adjudicated Deceased Donor AKI and Graft Outcomes [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/clinically-adjudicated-deceased-donor-aki-and-graft-outcomes/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress