Characterization of Donor/Recipient Citizenship Status in Adult Heart Transplantation: A UNOS Registry Analysis
1Keck Medicine of USC, Los Angeles, CA, 2Cardiology, Keck Medicine of USC, Los Angeles, CA, 3Cardiothoracic Surgery, Keck Medicine of USC, Los Angeles, CA, 4Newark Beth-Israel Medical Center, Newark, NJ, 5Harbor-UCLA Medical Center, Torrance, CA, 6University of Arizona Sarver Heart Center, Tucson, AZ, 7UCLA Medical Center, Los Angeles, CA, 8The Queen's Medical Center, Honolulu, HI
Meeting: 2020 American Transplant Congress
Abstract number: C-274
Keywords: Donation, Heart, Waiting lists
Session Information
Session Name: Poster Session C: Heart and VADs: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: There is a paucity of data describing heart transplant donor and recipient status. We therefore sought to examine the medical and demographic characteristics, and post-transplant outcomes based on donor & recipient citizenship status.
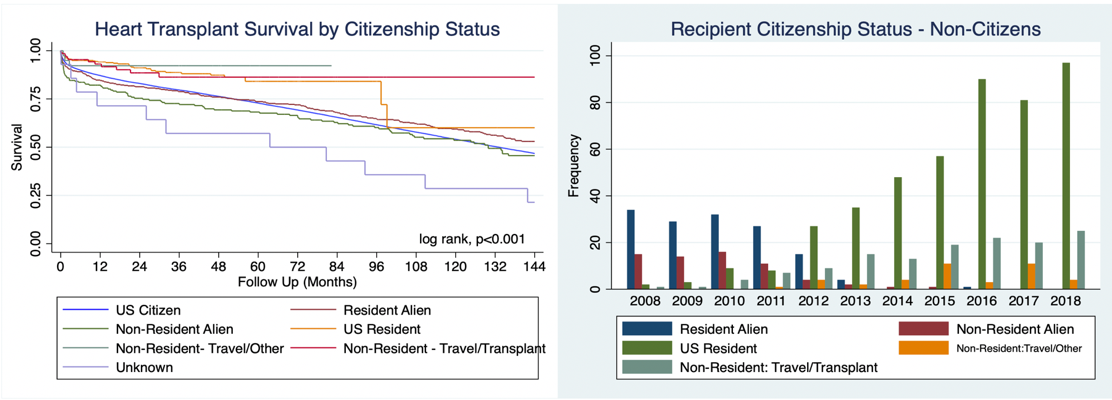
*Methods: We analyzed the UNOS registry for citizenship status, peri-transplant characteristics, and transplant outcomes of heart organ donors (n = 63,142) and recipients (n = 63,078), using a multivariate Cox proportional hazard regression model adjusting for age, sex, race, diabetes, ischemic time, need for dialysis/life support, and recipient wait-time. Kaplan Meier survival was censored at 10 years.
*Results: At transplant, age of US citizen recipients (46.7 ± 19.1) was higher than that of non-resident aliens (30.0 ± 21.4) and non-residents who traveled specifically for transplant (25.8 ± 22.6) (p<0.001). US citizens were more likely to have diabetes (20.6%) compared to non-resident aliens (9.6%) (p<0.001). Non-residents who traveled for transplant were more likely to be on IABP (11.6%), ECMO (2.2%), and VAD (36.2%) compared to US citizen recipients [IABP (5.5%), ECMO (1%), and VAD (24.9%)]. Non-residents traveling for non-transplant reasons (89.5 (IQR 21.5, 167.50 days) and US citizens ((83 (IQR 26, 231) days) had highest wait times. Compared to U.S. Census data, donors were less often white (69.5% vs 76.5%), Hispanic (13.5% vs 18.3%) or Asian, (1.4% vs 5.9%) and more often black (14.2% vs 13.4%). The majority of recipients (61,735/63,078 = 97.9%) and donors (59,945/63,142 = 95.1%) were US citizens.
*Conclusions: Non-residents who receive heart transplants are younger and require more mechanical circulatory support compared to US citizens. There was also a trend towards increased foreign travel for transplant. Additionally, there were fewer white, Hispanic, and Asian donors compared to the general population. Further study is warranted to understand this disparity and increase organ donation awareness among these communities.
To cite this abstract in AMA style:
Yang K, Miklin D, Pizula J, Genyk P, Liu G, Lee A, Nuno S, Hashmi S, Nattiv J, Kiankhooy A, Grazette L, Fong M, Rahman J, Pandya K, Vucicevic D, Li J, Kingsford P, Banankhah P, Chand R, Wolfson A, Shah S, Salimbangon A, Lum C, Depasquale EC, Vaidya AS. Characterization of Donor/Recipient Citizenship Status in Adult Heart Transplantation: A UNOS Registry Analysis [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/characterization-of-donor-recipient-citizenship-status-in-adult-heart-transplantation-a-unos-registry-analysis/. Accessed February 23, 2026.« Back to 2020 American Transplant Congress