Characterization of Acute Kidney Injury in Fatty Liver Ischemia Reperfusion Injury
Department of Surgery, Indiana University School of Medicine, Indianapolis, IN
Meeting: 2022 American Transplant Congress
Abstract number: 652
Keywords: Ischemia, Liver preservation, Renal dysfunction
Topic: Basic Science » Basic Science » 14 - Ischemia Reperfusion
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: The association between hepatic ischemia reperfusion injury (hIRI) and acute kidney injury (AKI) has been well established. AKI is commonly observed following transplantation of a steatotic graft. Using a murine hepatic IRI model, we sought to identify differences in kidney injury patterns between mice with lean and fatty livers.
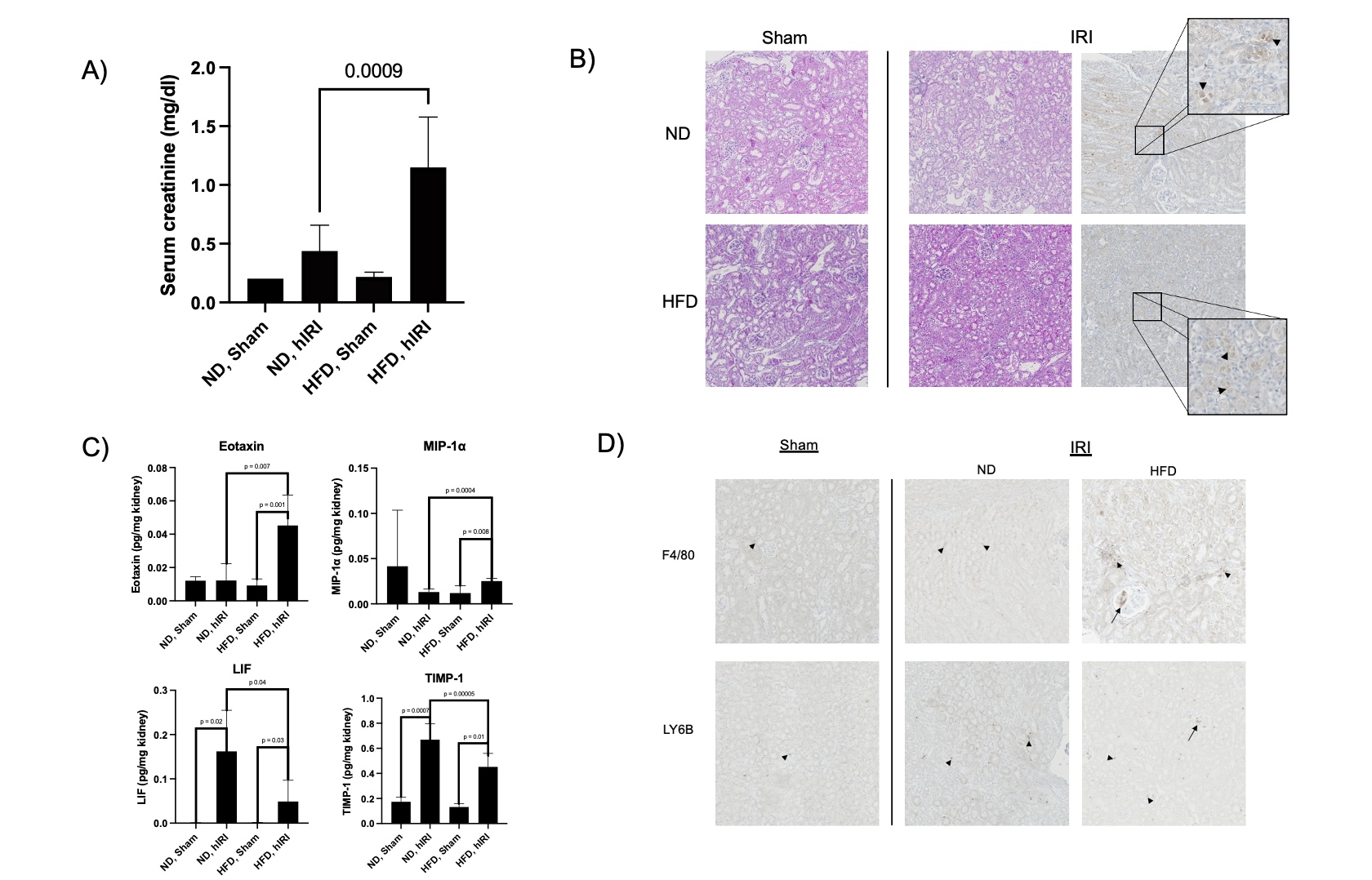
*Methods: 10-week-old C57BL6 male mice were split into two cohorts; one was fed high fat, high sucrose diet (HFD) (n = 8) for 12 weeks, while the other was maintained on normal chow diet (ND) (n = 8). At 22 weeks age, 4 animals from each group were subjected to hIRI with 70% portal pedicle clamping for 1 hour. Remaining mice underwent sham operations as controls. Following 24 hours of reperfusion mice were euthanized. Serum was analyzed for AST, ALT and creatinine. H&E staining and immunohistochemistry for cleaved caspase-3, F4/80, and LY6B were performed on kidney sections. Homogenized kidney tissue was used for Multi-plex cytokine discovery assay (Eve Technologies, Calgary, Canada).
*Results: Serum creatinine was significantly higher in HFD mice following liver IRI as compared to ND/hIRI mice (Figure 1-A). H&E staining demonstrated tubular epithelial sloughing in both HFD/hIRI and ND/hIRI kidneys. Cleaved caspase-3 staining was present in these sections as well (Figure 1-B). Multiplex cytokine analysis revealed increased levels of pro-inflammatory cytokines Eotaxin and Macrophage inflammatory peptide 1-alpha (MIP-1α) in HFD/hIRI kidneys as compared to ND/hIRI kidneys. Additionally, kidneys from HFD/hIRI mice had a lower concentrations of the anti-inflammatory cytokines Leukemia inhibitory factor (LIF) and Tissue inhibitor of metalloproteinase-1 (TIMP-1) compared to ND controls (Figure 1-C). F4/80 and LY6B IHC identified increased macrophage and neutrophil aggregation, respectively, following IRI. In HFD/hIRI kidneys, these inflammatory cells were also observed to localize to glomeruli (Figure 1-D). This pattern was not identified in ND/hIRI kidneys.
*Conclusions: Our data suggests a pro-inflammatory cytokine profile in kidneys after fatty liver IRI, potentially contributing to more severe AKI. The specific mechanisms of inflammation in the kidneys following fatty liver IRI remain to be elucidated.
To cite this abstract in AMA style:
Rokop ZP, Zhang W, Ghosh N, Das A, Biswas N, Sen C, Kubal C. Characterization of Acute Kidney Injury in Fatty Liver Ischemia Reperfusion Injury [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/characterization-of-acute-kidney-injury-in-fatty-liver-ischemia-reperfusion-injury/. Accessed March 3, 2026.« Back to 2022 American Transplant Congress