Characteristics and Outcomes of Patients with Cystic Fibrosis Receiving Lung Transplant with and without ECMO Bridge – A Single Center Experience
Pulmonary & Critical Care, USC, Los Angeles, CA
Meeting: 2020 American Transplant Congress
Abstract number: C-307
Keywords: Heart assist devices, Length of stay, Lung transplantation, Outcome
Session Information
Session Name: Poster Session C: Lung: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: ECMO is a viable bridge to lung transplantation (LTx) for end-stage cystic fibrosis (CF) patients refractory to traditional medical support. We sought to identify end-stage CF patients at risk for requiring ECMO as a bridge to LTx, and if there is a difference in morbidity or mortality when compared to those who received LTx without ECMO support.
*Methods: This is a single center retrospective chart review for all CF patients undergoing LTx from 2013-2018 (n=14). The cohort was divided into LTx with ECMO bridge (n=5) vs without ECMO bridge (n=9). A cohort of bridged patients who expired prior to LTx was also included for comparison (n=4).
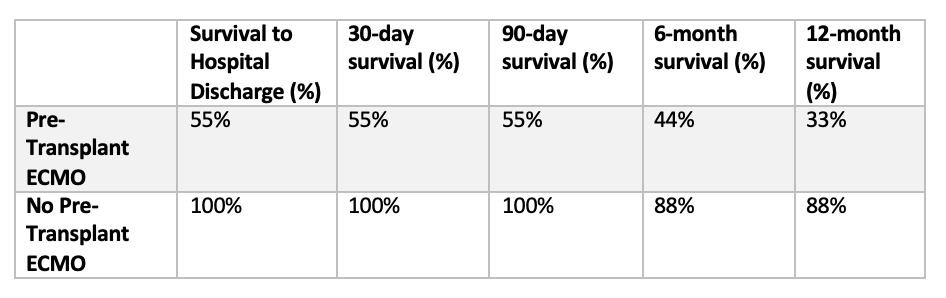
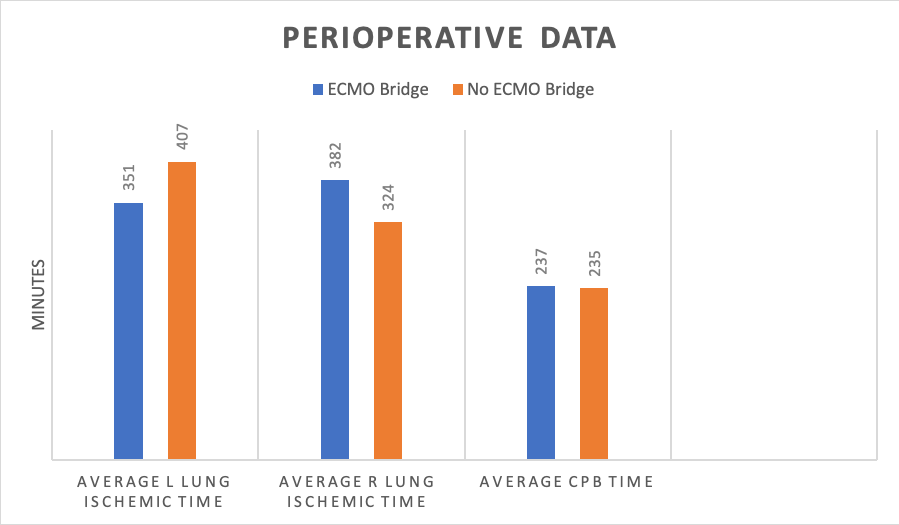
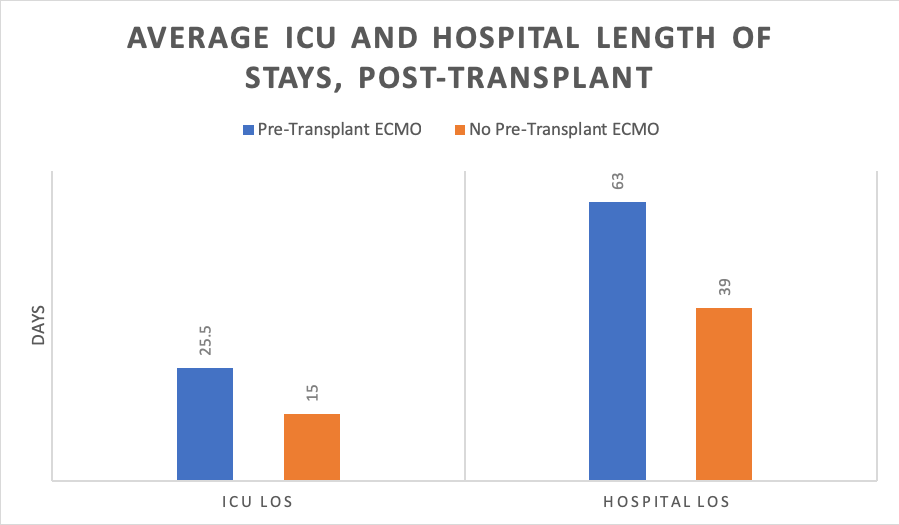
*Results: Average pre-LTx PaCO2 was 108mmHg in ECMO bridged patients, compared to 45mmHg in non-bridged patients. Number of pre-Tx mechanical ventilation (MV) days was higher in bridged patients. There was no difference in number of exacerbations prompting hospitalization in the 1 year preceding LTx. Rate of FEV1 decline was similar in both groups. There was no difference in intraoperative cardiopulmonary bypass time. For the ECMO group, average R lung ischemic time was higher (382m vs 324m), while average L lung ischemic time was lower (351m vs 405m). The ECMO group required more delayed chest closure (75% vs 22%). ICU and hospital LOS post-LTx was higher in the ECMO group. 88% of patients in the non-ECMO group survived to 1 year, whereas 6-mo and 1 year survival in the ECMO group was 44% and 33%, respectively.
*Conclusions: We propose using pre-transplant PaCO2 trend and MV days to earlier identify patients at risk for acute decompensation that may require ECMO support. The more classically used FEV1 trend may be a non-specific indicator of overall disease progression. Pre-LTx ECMO portends extended ICU and hospital LOS, increased early all-cause mortality, and, post-operatively, higher surgical morbidity.
To cite this abstract in AMA style:
Loeb J, Pirrotta S, Chung P, Ganesh S. Characteristics and Outcomes of Patients with Cystic Fibrosis Receiving Lung Transplant with and without ECMO Bridge – A Single Center Experience [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/characteristics-and-outcomes-of-patients-with-cystic-fibrosis-receiving-lung-transplant-with-and-without-ecmo-bridge-a-single-center-experience/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress