Center Variability in Organ Offer Acceptance and Waitlist Mortality in Lung Transplantation
1Duke University School of Medicine, Durham, NC, 2Department of Surgery, Duke University Medical Center, Durham, NC, 3Department of Biostatistics and Bioinformatics, Duke University School of Medicine, Durham, NC
Meeting: 2019 American Transplant Congress
Abstract number: 191
Keywords: Lung transplantation, Mortality, Outcome, Waiting lists
Session Information
Session Name: Concurrent Session: Setting the Table for Success after Lung Transplantation
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:18pm-5:30pm
Presentation Time: 5:18pm-5:30pm
Location: Room 206
*Purpose: Lung transplantation (LTx) offers a survival benefit for patients with end-stage lung disease. When suitable donors are identified, centers must accept or decline the offer for a matched candidate on their waitlist. The purpose of the study was to evaluate the degree to which center-level variability in organ acceptance impacts candidate survival.
*Methods: We performed a retrospective cohort study of candidates aged ≥ 12 waitlisted for isolated LTx in the US using UNOS/OPTN data from 5/2007-5/2017. Centers that never had candidates ranked first on a match run >10 times in a year were excluded. Logistic regression was fit to assess the relationship of offer acceptance with donor-, candidate-, and geographic factors. Listing center was evaluated as a fixed effect to determine the adjusted per-center acceptance rate. Competing risks analysis employing the Fine-Gray model was undertaken to ascertain the relationship between the adjusted per-center acceptance rate and waitlist mortality.
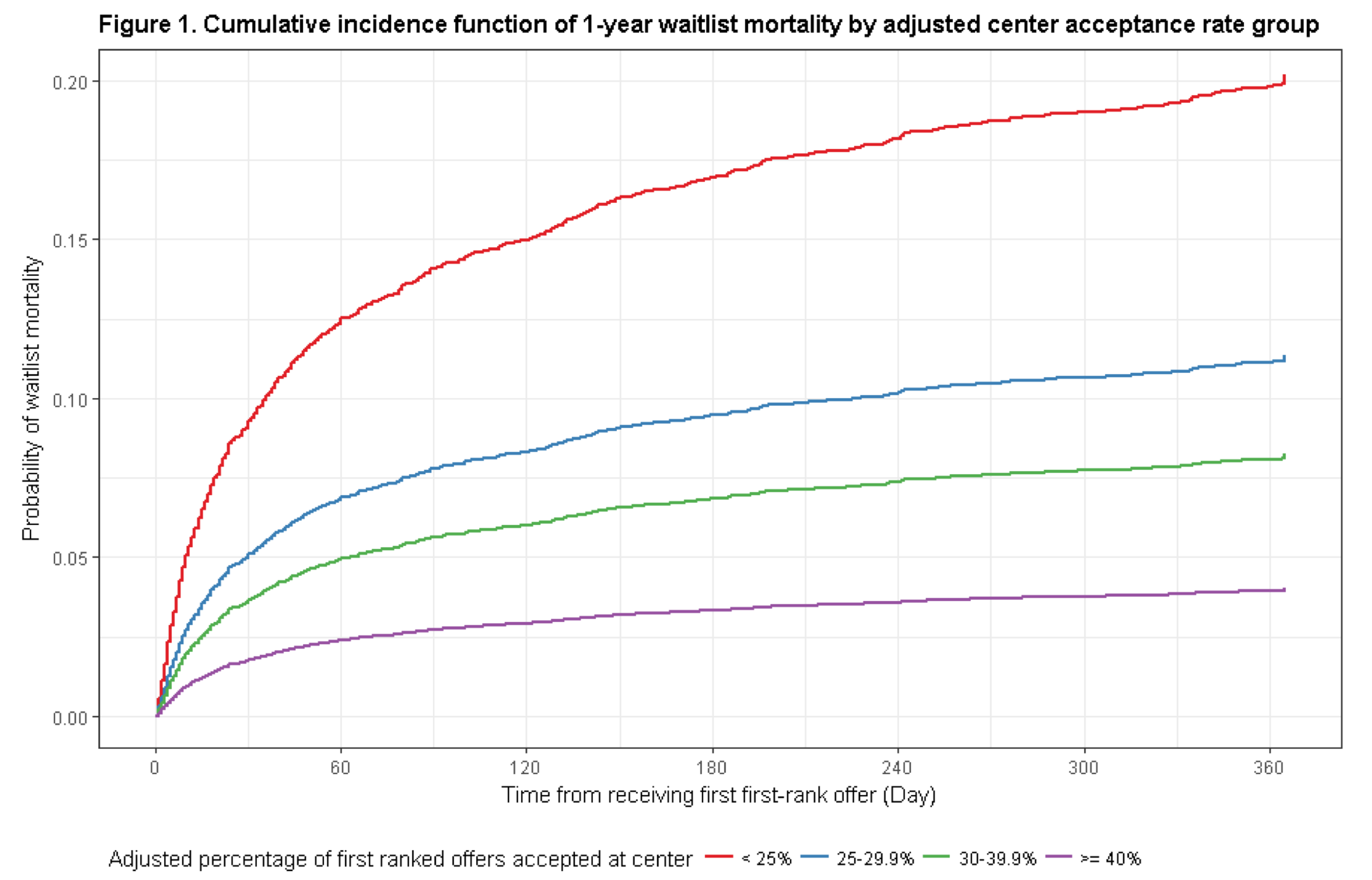
*Results: Of 15,847 unique organ offers, 4,735 (29.9%) were accepted for the first-ranked patients. After adjustment for important covariates, transplant centers varied markedly in acceptance rate practices (9% to 67%). Higher cumulative incidence of 1-year waitlist mortality was associated with lower acceptance rate (Figure 1). For every 10% increase in adjusted center acceptance rate, the risk of waitlist mortality decreased by 36.3% (subdistribution hazard ratio 0.637; CI 0.592, 0.685). Importantly, high-acceptance centers that accepted ≥ 40% of their first-ranked offers had improved 1-year posttransplant survival compared to centers with adjusted organ acceptance rates <25% (88.7% vs. 82.7%, log-rank test p=0.003).
*Conclusions: Variability in center-level behavior potentially represents the largest modifiable risk factor for prolonged waitlist times and mortality in LTx. Further intervention is needed to standardize center-level organ offer acceptance practices and minimize waitlist mortality at the national level.
To cite this abstract in AMA style:
Choi AY, Mulvihill MS, Weber J, Lee H, Cox M, Yerokun B, Kuchibhatla M, Klapper JA, Hartwig MG. Center Variability in Organ Offer Acceptance and Waitlist Mortality in Lung Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/center-variability-in-organ-offer-acceptance-and-waitlist-mortality-in-lung-transplantation/. Accessed February 15, 2026.« Back to 2019 American Transplant Congress