Better Never Than Late: Differences in Outcomes and Risk Factors for Early and Late Rejection After Kidney Transplantation.
Medicine, University Hospitals Case Medical Center, Cleveland, OH.
Meeting: 2016 American Transplant Congress
Abstract number: 509
Keywords: Graft failure, Kidney transplantation, Rejection
Session Information
Session Name: Concurrent Session: Kidney Transplant Recipient: Long Term Outcomes Session 2
Session Type: Concurrent Session
Date: Tuesday, June 14, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Ballroom A
Background: Late acute rejection (AR) is associated with inferior outcomes relative to early AR after kidney transplantation. We sought to examine the differences in risk factors for early AR (within 90 days of transplant) vs. late AR (occurring after one year post-transplantation).
Methods: We analyzed 500 consecutive solitary kidney recipients transplanted between 1/06 and 12/12. The cohort was 52% Caucasian and 43% African American (AA). All patients received tacrolimus/mycophenolate mofetil combination therapy, and corticosteroid withdrawal (CSW) was undertaken at day 5 in 320/491 (65%) of patients. Patients considered higher risk or with delayed function (DGF) were maintained on steroids (CSM). Death-censored allograft survival rates were examined and risk factors for early vs. late AR were identified by multivariable analysis.
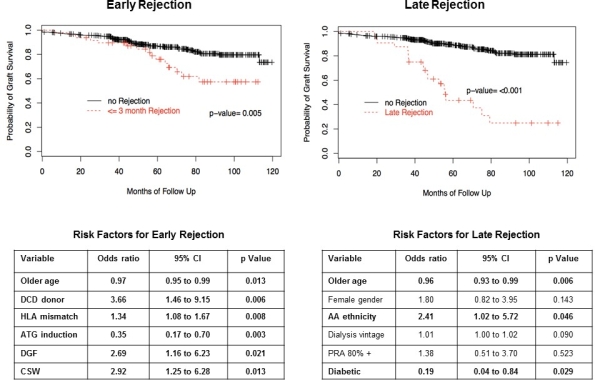
Results: Early and late AR occurred in 49/492 (10%) and 32/490 (7%) patients, respectively. There was no correlation between early and late AR (r= -0.3). Survival curves for early and late AR are shown below. Early AR did not affect immediate graft survival but ultimately contributed to graft loss after 4 years post-transplantation. Late AR had a greater negative impact on survival, with an 80% graft loss by 7 years. Risk factors associated with early and late AR by multivariable analyses are shown in the Tables. Donor after cardiac death (DCD) kidneys, DGF, HLA mismatching, and CSW were all risk factors for early AR. Older age and use of induction therapy with anti-thymocyte globulin were protective. Alternatively, AA ethnicity was a risk factor for late AR, while older age and diabetic status at transplantation appeared to be protective.
Conclusion: Both early and late AR negatively impact upon allograft survival, with a greater negative impact associated with late AR. Factors that predict early AR appear to have less bearing on late AR. Alternatively, AA ethnicity emerged as a risk for late AR, and may help to explain inferior outcomes identified in AA recipients. Given the high risk of allograft loss, it is critical to further assess the risk factors and causes of late AR after kidney transplantation.
CITATION INFORMATION: Liu A, Sarabu N, Joshua A. Better Never Than Late: Differences in Outcomes and Risk Factors for Early and Late Rejection After Kidney Transplantation. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Liu A, Sarabu N, Joshua A. Better Never Than Late: Differences in Outcomes and Risk Factors for Early and Late Rejection After Kidney Transplantation. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/better-never-than-late-differences-in-outcomes-and-risk-factors-for-early-and-late-rejection-after-kidney-transplantation/. Accessed February 21, 2026.« Back to 2016 American Transplant Congress
