Association of Belatacept Conversion on Patient and Allograft Survival in Kidney Transplant Recipients with Congestive Heart Failure
Department of Medicine, University of Wisconsin-Madison, Madison, WI
Meeting: 2021 American Transplant Congress
Abstract number: 938
Keywords: Co-stimulation, Echocardiography, Graft survival, Kidney transplantation
Topic: Clinical Science » Kidney » Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Information
Session Name: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Calcineurin inhibitors (CNI) exert deleterious effect on cardiovascular risk in kidney transplant recipients (KTRs). Belatacept conversion may reduce CV risk in KTRs. We hypothesized that early conversion to Belatacept will have better patient and graft survival and lower rate of readmission within 30-days in KTRs with congestive heart failure (CHF) compared to long-term CNI use.
*Methods: We merged Belatacept dataset in Wisconsin Allograft Recipient Database with Clarity Healthlink dataset which contain admitted recipients with CHF between 2014-2019 using ICD-10 Code I50 for CHF and E87.70 for volume overload. Subjects switching to Belatacept were divided into Early Conversion (EC: switched to Belatacept within one year from transplant) and Late Conversion (LC: switched after one year). The Greedy matching was used for the EC and LC participants based on transplant date in a 1:2 allocation ratio to CNI control subjects (CNI-c).
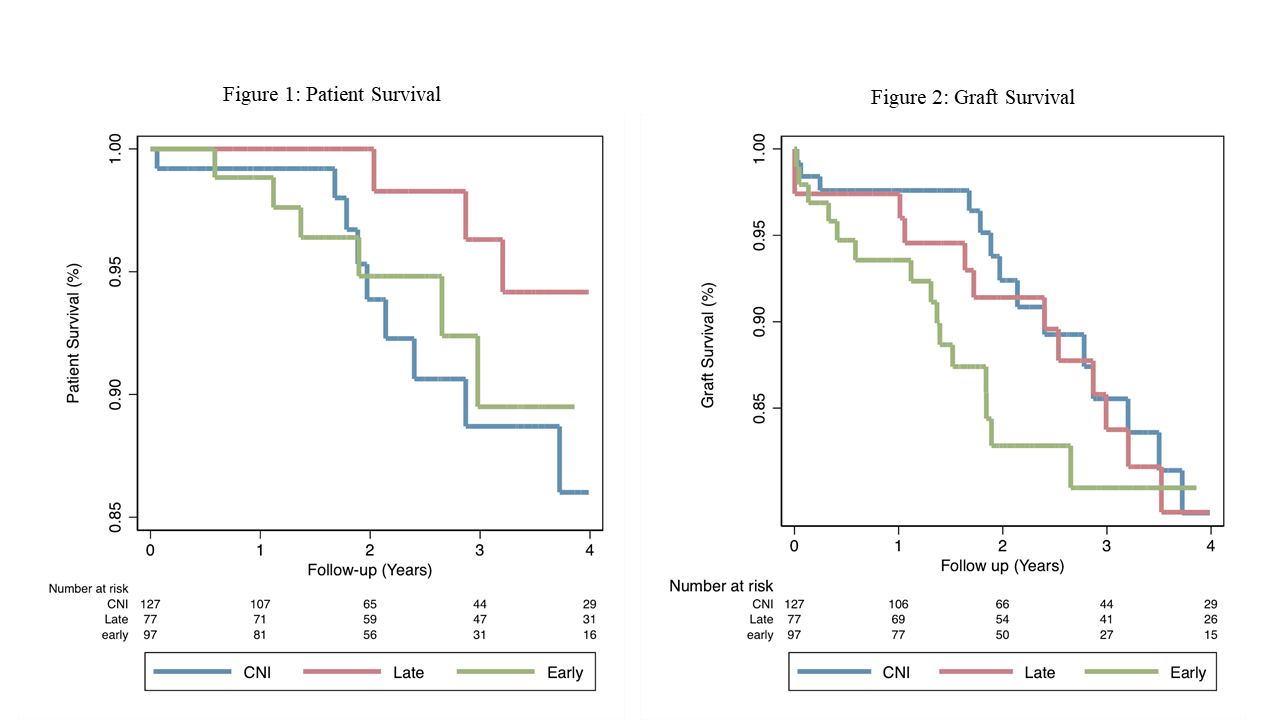
*Results: Of the 301 patients in the study, EC accounted for 31.5% (n=97), LC 25.1% (n=77), and CNI-c 43.3% (n=133). The median patient survival (years, IQR): CNI-c (2, 2.3), EC (2.2, 1.8) and LC (3.4, 2.4) (p<0.001). There was no significant difference in the prevalence of history of MI, CHF and CAD at time of transplant. Mean time to switching was 3.36 months and 3.5 years for EC and LC, respectively. Compared to Belatacept groups, CNI-c had significantly higher rate of Basiliximab induction (p=0.001), were more likely to have received deceased donor transplant (p=0.05) and had significantly younger donor age (43.2 years, p=0.04). Adjusted hazard ratios (aHR) showed no statistical difference for patient and graft survival between the three groups. However, conversion to Belatacept was associated with better numerical patient and graft survival (aHR 0.36, 95% CI [.03-3.8], p=0.4) and (aHR 0.74, 95% CI [0.1-7.2], P=0.8), respectively. There was no significant difference in readmission within 30-days rate (18%, 11% and 15%, p=0.32) among CNI-c, EC and LC, respectively.
*Conclusions: Patient and graft survival and rate of readmission within 30-days post CHF hospital discharge were not significantly different among the three groups. However, the patient and graft survival rates do suggest clinically protective effects of converting patients to Belatacept after transplant date.
To cite this abstract in AMA style:
Mogallapalli H. Association of Belatacept Conversion on Patient and Allograft Survival in Kidney Transplant Recipients with Congestive Heart Failure [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/association-of-belatacept-conversion-on-patient-and-allograft-survival-in-kidney-transplant-recipients-with-congestive-heart-failure/. Accessed March 7, 2026.« Back to 2021 American Transplant Congress