Allograft Discard Risk Index for Lung Transplantation
R. M. Reul, G. Loor, P. S. Garcha, A. A. Rana
Baylor College of Medicine, Houston, TX
Meeting: 2021 American Transplant Congress
Abstract number: 95
Keywords: Allocation, Donors, marginal, Lung transplantation, Outcome
Topic: Clinical Science » Lung » Lung: All Topics
Session Information
Session Name: How to Expect the Unexpected- Incorporating Predictors into Lung Transplant Decision Making
Session Type: Rapid Fire Oral Abstract
Date: Saturday, June 5, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:20pm-6:25pm
Presentation Time: 6:20pm-6:25pm
Location: Virtual
*Purpose: The demand for donor lungs continues to outpace the supply, yet nearly 80% of donor lungs consented for lung transplantation (LTx) are discarded.
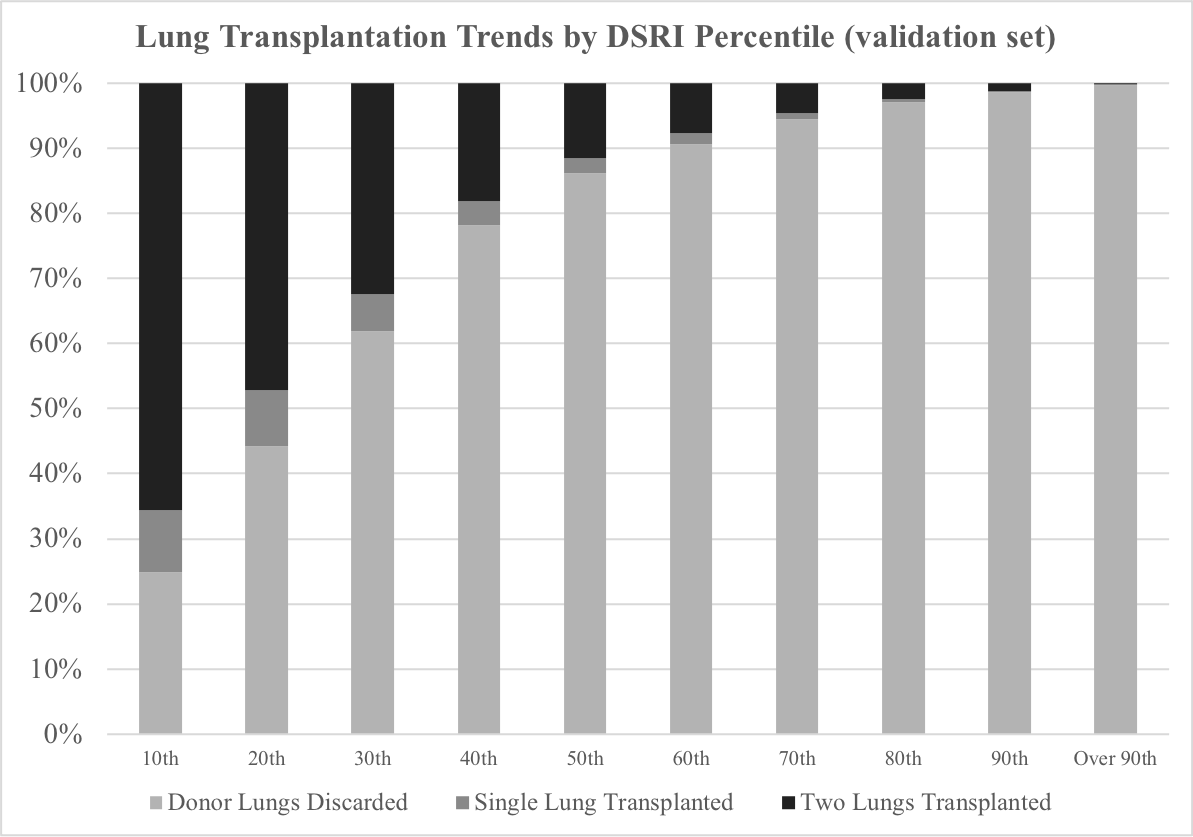
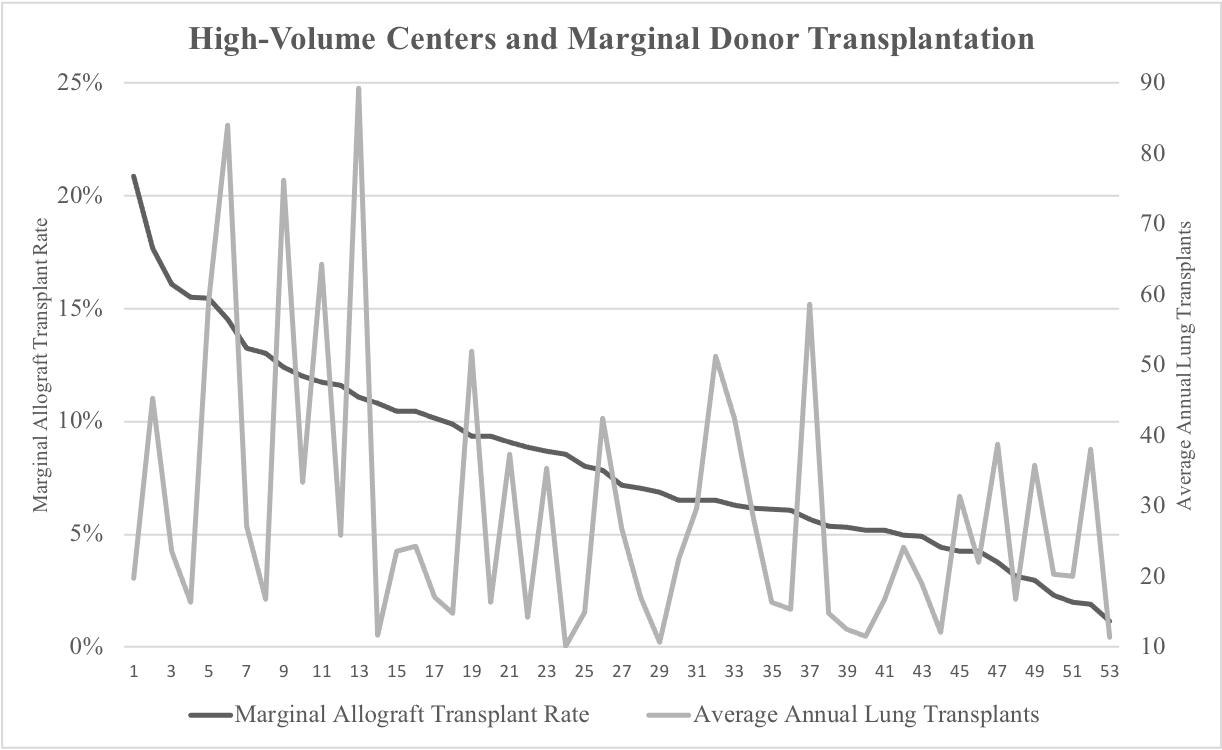
*Methods: We reviewed all deceased organ donors listed within the UNOS Deceased Donor Database between 2005 and 2015. Donors > 10 years old and consented for lung donation were included in our analysis. Univariate and multivariate analyses were run on the training set (n=80,614) with the primary outcome of lung discard, and the results were used to create a discard risk index (DSRI). Discard data was assessed at DSRI value deciles using the validation set (n=40,306), and differences in 1-year mortality were assessed using stratum-specific likelihood ratio (SSLR) analysis. Marginal donors were defined as the top 50 percentiles of DSRI values for a high-volume center analysis.
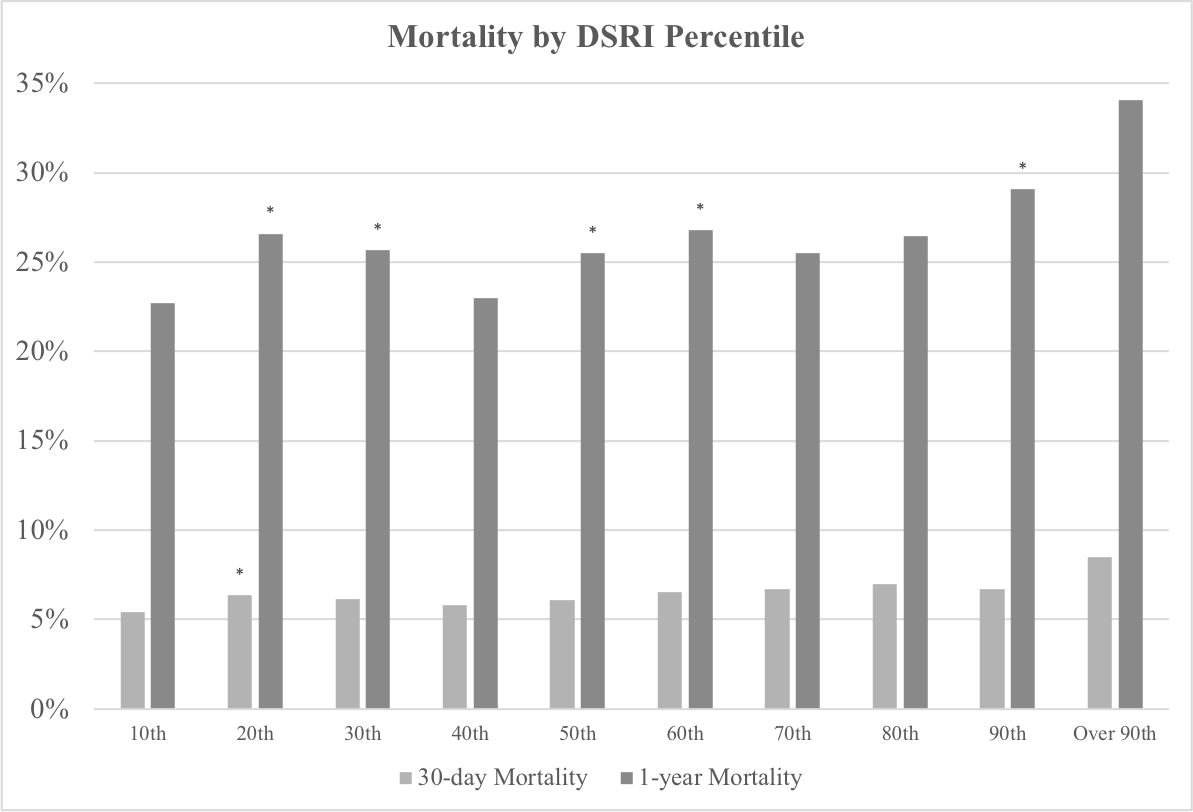
*Results: Donor factors most associated with higher DSRI values included age > 65, PaO2 < 300 on 100% FiO2, HCV, and cigarette use. Factors associated with lower DSRI values included donor age < 40, and PaO2 > 400. The DSRI was a reliable predictor of donor discard, with a C-statistic of 0.870 in the training set and 0.873 in the validation set. The DSRI was not a reliable predictor of 30-day or 1-year survival following transplantation (C-statistic of 0.520 & 0.518, respectively). SSLR analysis resulted in just two 1-year mortality strata (SSLR 0.89 in the 1st DSRI value decile & 1.06 in the 2nd-10th). Analysis of high-volume centers (>10 LTx per year) revealed substantial variation in the amount of marginal donor transplants by de-identified center.
*Conclusions: The factors leading to lung allograft discard are not the same as those leading to beneficial outcomes. This suggests that with proper allocation, grafts that would have been historically discarded could be used in the future donor pool with limited impact on mortality.
To cite this abstract in AMA style:
Reul RM, Loor G, Garcha PS, Rana AA. Allograft Discard Risk Index for Lung Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/allograft-discard-risk-index-for-lung-transplantation/. Accessed February 22, 2026.« Back to 2021 American Transplant Congress