Allograft Discard Risk Index for Heart Transplantation
1Office of Student Affairs, Baylor College of Medicine, Houston, TX, 2Michael E. DeBakey Department of Surgery, Baylor College of Medicine, Houston, TX
Meeting: 2021 American Transplant Congress
Abstract number: 46
Keywords: Donors, marginal, Graft acceptance, Heart transplant patients, Risk factors
Topic: Clinical Science » Heart » Heart and VADs: All Topics
Session Information
Session Name: Heart: Triple "D" in Heart Transplantation: DCD, Dual-Organ and Declined Hearts
Session Type: Rapid Fire Oral Abstract
Date: Saturday, June 5, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 4:45pm-4:50pm
Presentation Time: 4:45pm-4:50pm
Location: Virtual
*Purpose: The number of patients awaiting heart transplantation (HTx) substantially exceeds the number of donor hearts transplanted each year, yet nearly 70% of consented donor hearts are discarded rather than transplanted.
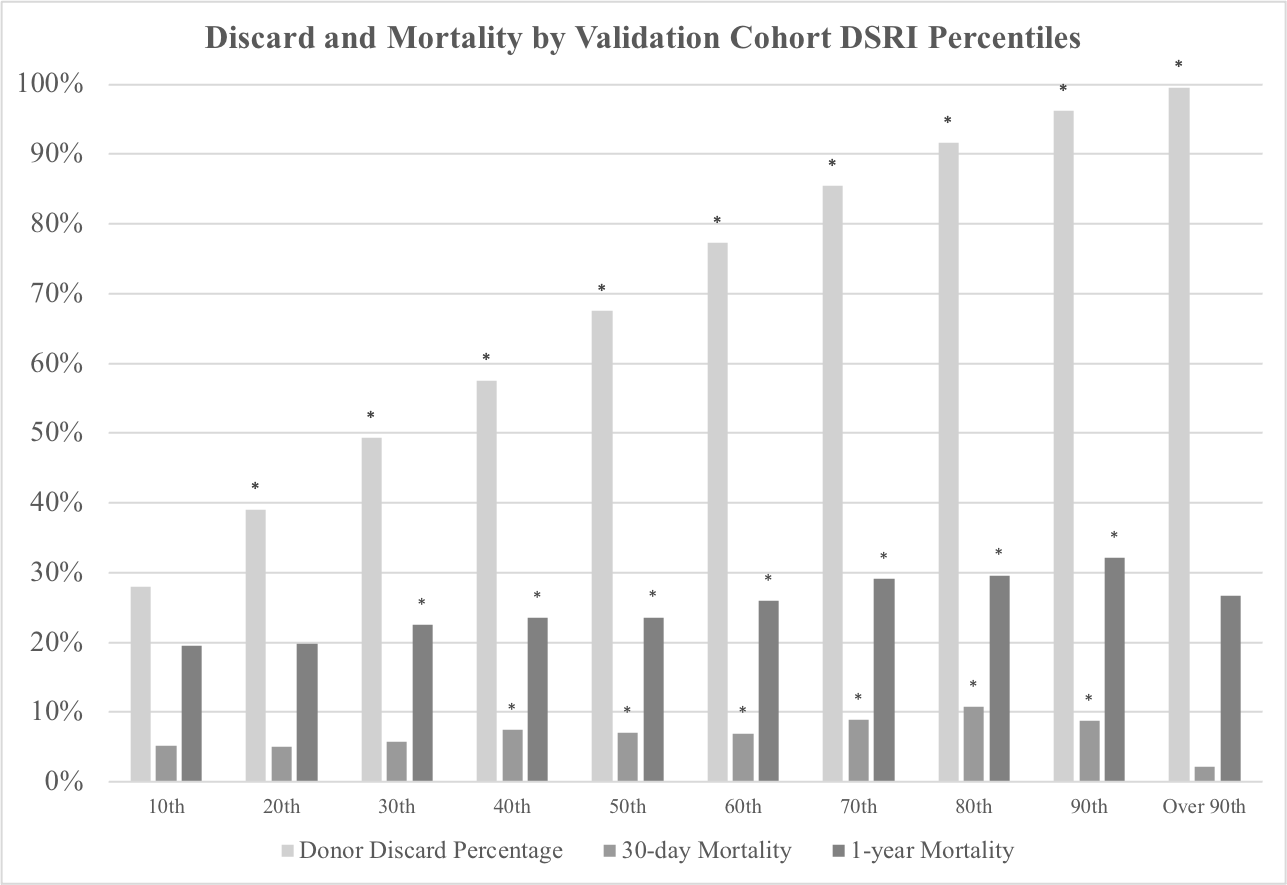
*Methods: All deceased organ donors listed within the UNOS Deceased Donor Database between June 12, 2005 and June 12, 2020 were reviewed. Those greater than 10 years old and consented for heart donation were included and randomly separated into training (n=79,704) and validation (n=39,852) cohorts. Demographic factors were compared between groups. A univariate and multivariate analysis was run on the training set to determine factors significant for allograft discard. Those factors were then used to create the discard risk index (DSRI). Discard and mortality data were assessed at DSRI value deciles using the validation set, and stratum-specific likelihood ratio (SSLR) analysis was used to determine deciles with increased likelihood of 1-year mortality.
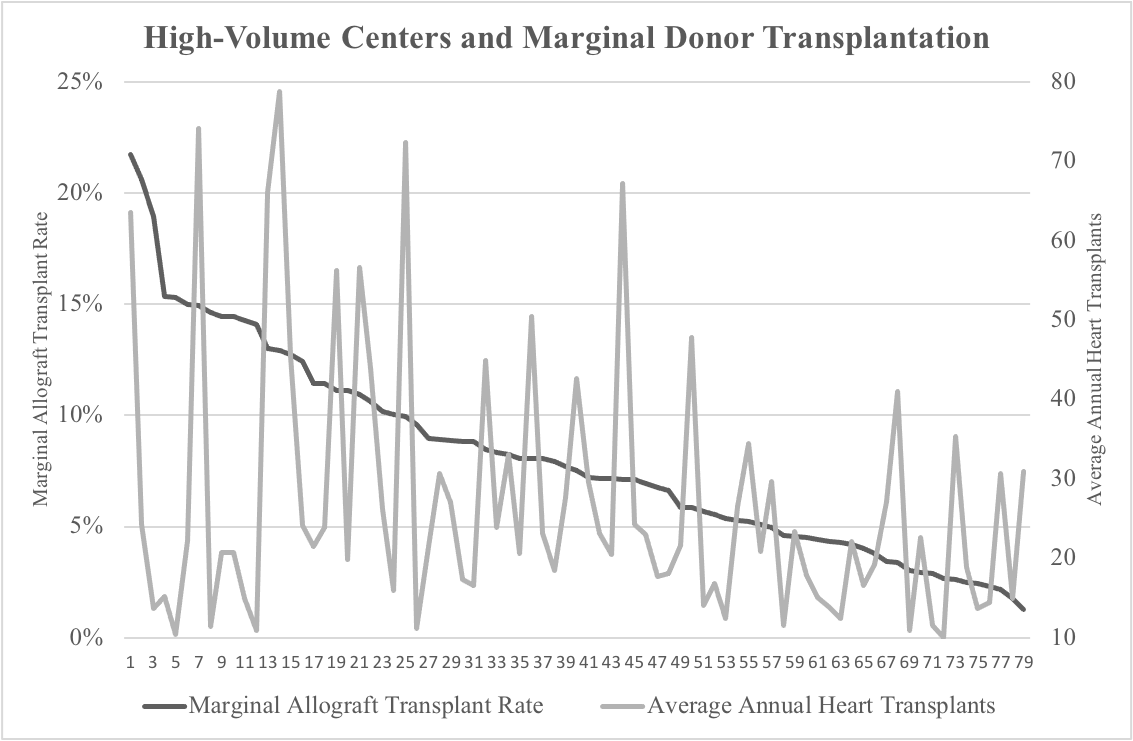
*Results: Factors associated with higher DSRI values included donor age > 45, HCV or HBV-core antibodies, hypertension, diabetes, and prior myocardial infarction. Factors associated with lower DSRI values included donor age < 40 and trauma as the donor cause of death. The DSRI C-statistic was 0.821 in the training cohort and 0.819 in the validation cohort. The DSRI did not reliably predict 30-day or 1-year mortality after transplantation (C-statistic 0.557 & 0.546, respectively). The highest SSLR for 1-year mortality was the top 4 DSRI deciles (SSLR 1.46). This group was used to define marginal donors. An analysis of high-volume centers (10 or more HTx per year) resulted in substantial variation in terms of marginal donor usage.
*Conclusions: The factors leading to heart allograft discard have little correlation with post-transplant outcomes. This suggests that with proper allocation, allografts at higher risk for discard may be transplanted with limited impact on recipient mortality.
To cite this abstract in AMA style:
Reul RM, Saleem AA, Keller CN, Malik TH, Goss JA, Rana AA. Allograft Discard Risk Index for Heart Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/allograft-discard-risk-index-for-heart-transplantation/. Accessed February 25, 2026.« Back to 2021 American Transplant Congress