Age Should Not Be Considered a Contraindication for Living Kidney Donation
Imperial College Renal and Transplant Centre, Hammersmith Hospital, London, United Kingdom.
Meeting: 2015 American Transplant Congress
Abstract number: C153
Keywords: Age factors, Donation, Elderly patients, Kidney transplantation
Session Information
Session Name: Poster Session C: Living Donor Issues 2
Session Type: Poster Session
Date: Monday, May 4, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
The increasing numbers of patients with ESRD on the transplant waiting list has been the main driving force for expanding the donor pool. Acceptance of elderly living donors remains controversial because of the higher incidence of comorbities.We undertook living kidney donor transplantation from elderly donors after reports that short-term outcomes are safe. We report 5-yr data and compare these with the outcomes of younger donors.
Data was prospectively collected on 553 consecutive live donors from 2000-2012. Donors were categorized in two age groups: <60 years (younger) and ≥60 years (elderly). We analysed 5-yr follow-up data for kidney function [Creatinine Clearance (CrCl)] and protein excretion as well as blood pressure control.
83 donors were ≥60 years and 470 were <60 years. 62 (74.7%) in the group of elderly donors were Caucasians (CA) .Overall, in the total donor population, 18.4% of the CA were elderly, while 10.6% of South Asians and 2% of AfroCaribbeans were elderly .There was no difference regarding gender (60.2% female in elderly vs 55.5% in younger, p=0.425). There were more Caucasians (p=0.008) and more hypertensive in the elderly group (19.3% versus 7.4%, p=0.001). Elderly group had lower CrCl pre-donation (98.6±22 vs 112±33, p<0.001). There was no difference in BMI or proteinuria.
The CrCl at 5 years was 78.7±16 in elderly and 91.6±27 mls/min in younger donors (p=0.067). Decline of CrCl was similar in both groups. 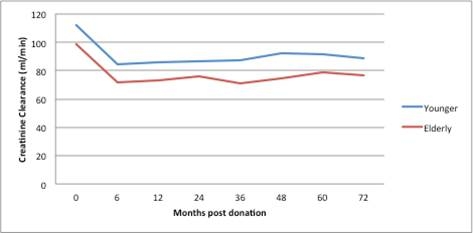 There was no significant proteinuria at 5 years (Elderly=0.12±0.1, Younger=0.12±0.6 g/24hrs, p=0.872). Blood pressure remained well-controlled at 5 years at 133/77 (elderly) vs 136/82 (younger) (p=0.384 and 0.07). 13 (15.7%) elderly and 30 (6.4%) younger donors developed post-donation HTN (p=0.001).
There was no significant proteinuria at 5 years (Elderly=0.12±0.1, Younger=0.12±0.6 g/24hrs, p=0.872). Blood pressure remained well-controlled at 5 years at 133/77 (elderly) vs 136/82 (younger) (p=0.384 and 0.07). 13 (15.7%) elderly and 30 (6.4%) younger donors developed post-donation HTN (p=0.001).
We conclude that donor nephrectomy in carefully selected elderly donors seems to be safe. There was no difference in CrCl trends among elderly and younger donors and proteinuria was minimal over 5 years. Long-term follow up of donors remains important enabling identification of patients at risk of declining renal function or hypertensive complications.
To cite this abstract in AMA style:
Moutzouris D-A, Charif R, Galliford J, McDermott J, Dulku H, Orr H, Taube D, Loucaidou M. Age Should Not Be Considered a Contraindication for Living Kidney Donation [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/age-should-not-be-considered-a-contraindication-for-living-kidney-donation/. Accessed March 7, 2026.« Back to 2015 American Transplant Congress
