Adult-Sized Kidneys Transplanted into Infants and Small Children: Outcomes after Implementing Aggressive Fluid Regimen and Medications to Support Post-Transplant Perfusion
Lucile Packard Children's Hospital, Palo Alto, CA.
Meeting: 2018 American Transplant Congress
Abstract number: B243
Keywords: Kidney transplantation, Pediatric
Session Information
Session Name: Poster Session B: Kidney: Pediatrics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background: Risk of chronic graft ischemia secondary to hypoperfusion increases with greater disparity between donor and recipient size. At our center, the smallest recipients receive aggressive fluid and medication regimens to support blood pressure (BP) and allograft blood flow post-transplant. The goal is to provide adequate perfusion of the adult-sized kidney to preserve graft function.
Methods: Study design was retrospective chart review. Inclusion criteria: 1) children with BSA<0.75 m2, receiving an adult donor renal transplant between JAN 2006-AUG 2016, 2) minimum 1 year followup, 3) adequate 1-year protocol renal allograft biopsy. Exclusion criteria included; clinical rejection episode. BP trend was estimated averaging home BP logs and clinic visits. A group of 28 patients, transplanted between 1999-2006 with less aggressive BP maintenance, served as a historical control. GFR estimate was by corrected Schwartz method. The same pathologists reviewed all biopsies.
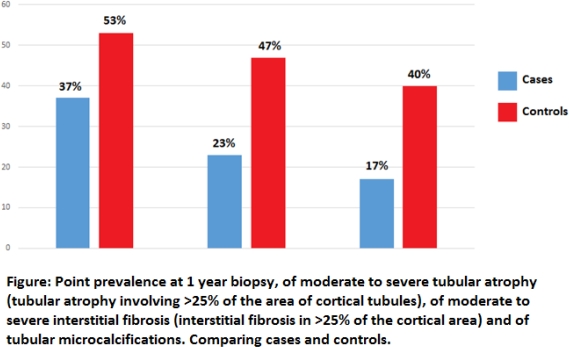
Results: 305 patients were identified, 30 met inclusion criteria. Age (median (range)) at transplant was 2 (1-5) years , weight 14.0(10.1-20.5) kg, BSA 0.56 (0.45-0.74) m2 and 33% received deceased donor kidney. All patients received hydration of 2500 ml/m2/day during the first year. All received 1 or more medications, 18 fludrocortisone, 21 NaCl supplements and 11 midodrine. BP percentile average over 12 months was >90% in 21 patients. Despite treatment, 9 remained normotensive. Echocardiogram results were available for 13 (43%), of those 2 had LVH. Both had BP trend >99%. At 1 year mean eGFR was 103 ±27, compared to 86±26 in the control group, p =0.025. Figure shows the 1 year prevalence of tubular atrophy, interstitial fibrosis and tubular microcalcifications in cases and controls.
Conclusion: Aggressive post-transplantation management strategies to increase allograft perfusion focusing on BP support and maintenance of recipient intravascular volume have improved allograft function and decreased ischemic injury to the transplanted kidney. This is achieved with minimal early cardiovascular morbidity.
CITATION INFORMATION: Sigurjonsdottir V., Grimm P., Chaudhuri A. Adult-Sized Kidneys Transplanted into Infants and Small Children: Outcomes after Implementing Aggressive Fluid Regimen and Medications to Support Post-Transplant Perfusion Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Sigurjonsdottir V, Grimm P, Chaudhuri A. Adult-Sized Kidneys Transplanted into Infants and Small Children: Outcomes after Implementing Aggressive Fluid Regimen and Medications to Support Post-Transplant Perfusion [abstract]. https://atcmeetingabstracts.com/abstract/adult-sized-kidneys-transplanted-into-infants-and-small-children-outcomes-after-implementing-aggressive-fluid-regimen-and-medications-to-support-post-transplant-perfusion/. Accessed June 30, 2025.« Back to 2018 American Transplant Congress