Acute Kidney Injury in Deceased Organ Donors and Kidney Transplant Outcomes Using a Novel Data Source
Perelman School of Medicine, University of Pennsyl, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: 335
Keywords: Donors, marginal, Kidney transplantation
Session Information
Session Name: Kidney Deceased Donor Selection II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:27pm-3:39pm
Presentation Time: 3:27pm-3:39pm
Location: Virtual
*Purpose: The kidney shortage necessitates innovative approaches to expand the donor pool. Acute kidney injury(AKI) is common among deceased donors and a risk factor for discard.
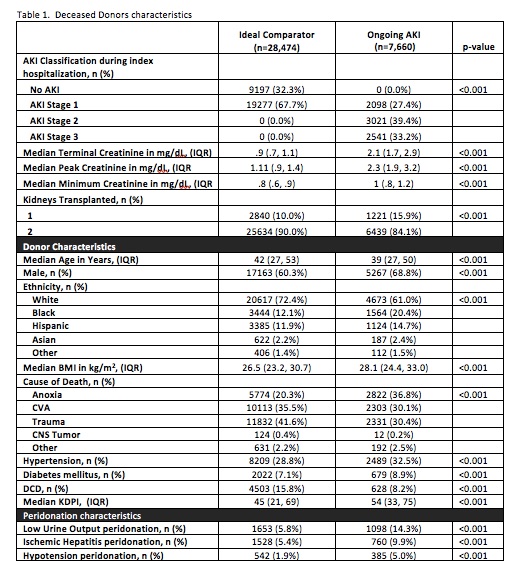
*Methods: Using a comprehensive OPTN and DonorNet dataset, we studied adult kidney-only recipients of donors with AKI between 5/2007-12/2016. DonorNet was used to characterize longitudinal creatinine changes, urine output, and other donor attributes during the terminal hospitalization. Donor AKI was defined as KDIGO AKI stage 1 or higher and terminal creatinine≥1.5mg/dL. Outcomes of kidney transplants from donors with AKI were compared to donors with no/resolved AKI stage 1 and a terminal creatinine<1.5mg/dL (termed the “ideal comparators”). We fit hierarchical linear regression models and proportional hazards frailty models for the primary outcomes of all-cause graft failure(GF) and 12-month estimated glomerular filtration rate(eGFR).
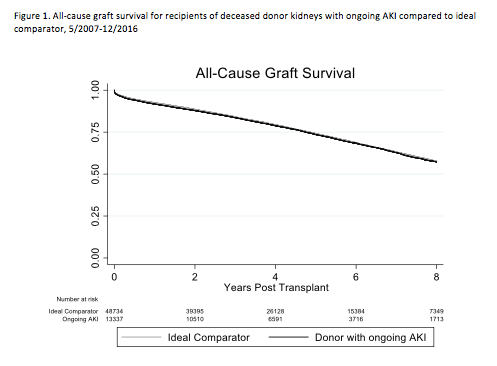
*Results: We identified 7,660 donors with ongoing AKI (33.2% with AKI stage 3, Table 1). Unadjusted rates of all-cause GF within 3 years were similar (15.5% in AKI donors vs 15.1% in ideal comparator, p=0.2, Figure 1). After risk adjustment, there was a slight elevation in all-cause GF among recipients of AKI kidneys (aHR 1.05, 95%CI: 1.01-1.09, Table 2). Mean 12-month eGFR was lower, but differences were not clinically important, among recipients of AKI kidneys (56.6 vs 57.5mL/min/1.73m2; p<0.001). Results were similar after risk-adjustment (Table 2). There were 3,950 discarded kidneys from donors with AKI, age≤65, without hypertension or diabetes, and terminal creatinine≤4.
*Conclusions: Among transplants performed in the US, grafts from donors with AKI have clinically similar graft function and failure rates. Donors with AKI offer an opportunity to substantially expand kidney transplantation.
To cite this abstract in AMA style:
Sonnenberg EM, Hsu J, Cohen J, Potluri V, Levine MH, Abt PL, Reese PP. Acute Kidney Injury in Deceased Organ Donors and Kidney Transplant Outcomes Using a Novel Data Source [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/acute-kidney-injury-in-deceased-organ-donors-and-kidney-transplant-outcomes-using-a-novel-data-source/. Accessed July 3, 2025.« Back to 2020 American Transplant Congress