Acute Kidney Injury and Chronic Kidney Disease in Donation After Circulatory Death Liver Transplantation: UK Single Centre Study.
1The Liver Unit, Queen Elizabeth Hospital, Birmingham, United Kingdom
2Nephrology and Dialysis Unit, Sapienza University of Rome, Rome, Italy
3Department of Health Informatics, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
4Department of Nephrology and Transplantation, Queen Elizabeth Hospital, Birmingham, United Kingdom
5NIHR Birmingham Liver Biomedical Research Unit and Centre for Liver Research, University of Birmingham, Birmingham, United Kingdom.
Meeting: 2016 American Transplant Congress
Abstract number: 81
Keywords: Donors, Liver transplantation, non-heart-beating, Post-operative complications, Renal dysfunction
Session Information
Session Name: Concurrent Session: The Kidney in Liver Transplantation
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Room 302
Aim of the study is to assess the incidence of acute kidney injury (AKI) and chronic kidney disease (CKD) after liver transplantation (LT) in DCD vs. DBD recipients.
Methods: this is a retrospective single-centre study of 1151 patients who underwent LT from 2007 to 2014. Exclusion criteria: urgent (=66) and living donor (=7) LT. We considered: renal function pre-LT, daily within one week post-operatively, at 1, 3, 4, 6, 9 months and 1, 3, 5 years post-LT, characteristics of recipient, donor type, graft variables and indicators of initial graft function. AKI and CKD defined and classified on the basis of KDIGO Guidelines (2012).
Results: we considered 1078 LT patients (830 DBD and 248 DCD). DBD recipients had a higher MELD (p=0.002) and pre-LT serum bilirubin level (p<0.001) than DCD but there were no differences in INR and serum creatinine values. DBD recipients had longer cold and recipient warm ischemia times than DCD (p<0.001 and p=0.018 respectively). The incidence of AKI was 57.9% (624/1078), of which 57.1% of DBD (474/830) vs. 60.5% of DCD (150/248). DCD recipients had a higher incidence of stage 3 AKI than DBD (20.6% vs. 12.7%, p=0.0197). Among patients with stage 3 AKI DCD had a higher cumulative incidence of CKD compared to DBD (SHR 1.6 (1.0-2.7), p=0.051). 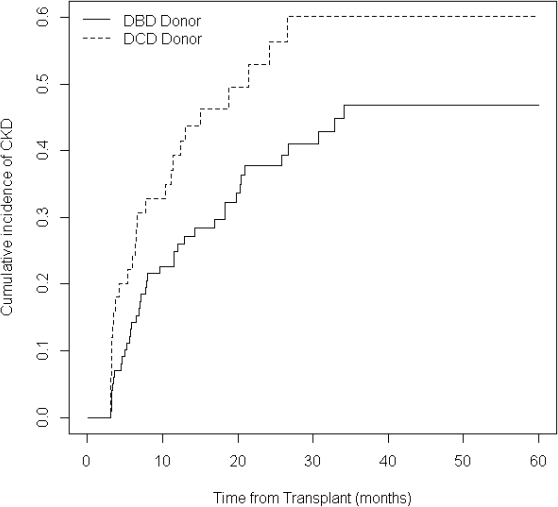
Conclusion: For the first time we showed that both DBD and DCD recipients suffer a similar degree of stage 1-2 of AKI, but the DCD experience more severe stage 3 AKI, which is associated with a higher incidence of CKD in the long-term follow-up.
CITATION INFORMATION: Umbro I, Tinti F, Evison F, Sharif A, Gunson B, Mitterhofer A, Ferguson J, Muiesan P. Acute Kidney Injury and Chronic Kidney Disease in Donation After Circulatory Death Liver Transplantation: UK Single Centre Study. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Umbro I, Tinti F, Evison F, Sharif A, Gunson B, Mitterhofer A, Ferguson J, Muiesan P. Acute Kidney Injury and Chronic Kidney Disease in Donation After Circulatory Death Liver Transplantation: UK Single Centre Study. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/acute-kidney-injury-and-chronic-kidney-disease-in-donation-after-circulatory-death-liver-transplantation-uk-single-centre-study/. Accessed February 24, 2026.« Back to 2016 American Transplant Congress
