A Novel Dropout Risk Score in Hepatocellular Carcinoma (HCC) Patients Listed for Liver Transplant (LT) – Identifying a Threshold That Predicts Worse Post-LT Survival in Short Wait Regions
UCSF, San Francisco.
Meeting: 2018 American Transplant Congress
Abstract number: 353
Keywords: Malignancy, Outcome
Session Information
Session Name: Concurrent Session: Liver: MELD, Allocation and Donor Issues - 1
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:54pm-5:06pm
Presentation Time: 4:54pm-5:06pm
Location: Room 6B
Background: Short wait time to LT for HCC patients may result in transplanting aggressive tumors at high risk for HCC recurrence who otherwise would have experienced dropout with longer wait time. We aimed to create a dropout risk score among HCC patients listed in long wait regions (LWR) and to apply this score in short wait regions (SWR) to evaluate post-LT outcomes. We hypothesized that receiving LT in SWR with a dropout risk score beyond a certain threshold would result in poor post-LT outcome. Methods: Using the UNOS database, we identified 2,092 adult HCC patients in LWR (Regions 1,5,9) and 1,735 in SWR (3,10,11) who received priority listing from 2010-2014. The dropout risk score was created in LWR patients using the multivariable competing risk regression coefficients of listing variables that predicted waitlist dropout. Results: Cumulative incidence of dropout in LWR within 1 year of priority listing was 18.6% (95% CI 16.9-20.3). On multivariable analysis of LWR patients, 1 tumor 3.1-5 cm or 2-3 tumors, AFP >20 ng/ml and increasing Child-Pugh and MELD-Na scores significantly predicted waitlist dropout. These 4 variables were used in the dropout risk score (C-statistic 0.74).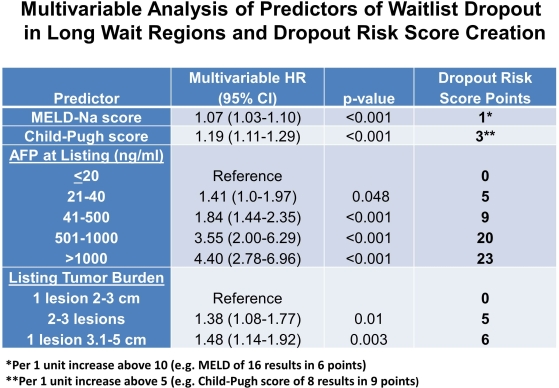 The median dropout risk score was 14 (IQR 7-23) in LWR and 16 (IQR 9-25) in SWR (p<0.001). In LWR, the dropout risk score stratified 1-year cumulative incidence of dropout ranging from 7.1% with a score <7 (lowest dropout risk quartile) to 40% with a score >23 (highest risk quartile). Cumulative incidence of LT within 1 year of priority listing in SWR was 89% at a median of 2.2 months from listing. When applying the dropout risk score to patients receiving LT in SWR, 5-year Kaplan-Meier post-LT survival with a dropout risk score <30 (n=1259) was 72% compared with 60% for a score >30 (n=191) (p=0.004). Conclusion: We developed a novel HCC dropout risk score which stratified 1-year dropout risk in LWR from 7% up to 40%. Patients in SWR with a dropout risk score >30 who received LT in part due to short wait time had inferior post-LT survival. This score may be useful in prioritizing organ allocation to HCC patients who would derive the greatest LT benefits.
The median dropout risk score was 14 (IQR 7-23) in LWR and 16 (IQR 9-25) in SWR (p<0.001). In LWR, the dropout risk score stratified 1-year cumulative incidence of dropout ranging from 7.1% with a score <7 (lowest dropout risk quartile) to 40% with a score >23 (highest risk quartile). Cumulative incidence of LT within 1 year of priority listing in SWR was 89% at a median of 2.2 months from listing. When applying the dropout risk score to patients receiving LT in SWR, 5-year Kaplan-Meier post-LT survival with a dropout risk score <30 (n=1259) was 72% compared with 60% for a score >30 (n=191) (p=0.004). Conclusion: We developed a novel HCC dropout risk score which stratified 1-year dropout risk in LWR from 7% up to 40%. Patients in SWR with a dropout risk score >30 who received LT in part due to short wait time had inferior post-LT survival. This score may be useful in prioritizing organ allocation to HCC patients who would derive the greatest LT benefits.
CITATION INFORMATION: Mehta N., Dodge J., Yao F. A Novel Dropout Risk Score in Hepatocellular Carcinoma (HCC) Patients Listed for Liver Transplant (LT) – Identifying a Threshold That Predicts Worse Post-LT Survival in Short Wait Regions Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Mehta N, Dodge J, Yao F. A Novel Dropout Risk Score in Hepatocellular Carcinoma (HCC) Patients Listed for Liver Transplant (LT) – Identifying a Threshold That Predicts Worse Post-LT Survival in Short Wait Regions [abstract]. https://atcmeetingabstracts.com/abstract/a-novel-dropout-risk-score-in-hepatocellular-carcinoma-hcc-patients-listed-for-liver-transplant-lt-identifying-a-threshold-that-predicts-worse-post-lt-survival-in-short-wait-regions/. Accessed January 1, 2026.« Back to 2018 American Transplant Congress
